Jan 11, 2019
The Stroke Alliance for Europe (SAFE), participates in EU funded research projects. Our involvement in research allows us to stay up-to-date on the latest research breakthroughs and promising treatments and to ensure that this potential live-saving knowledge reaches patients and healthcare professionals all across Europe. Our major strength is dissemination.
This video contains updates from five research projects that SAFE is actively involved in and these information have already been translated to Greek language by the Cyprus Stroke Organisation and the Hellenic Alliance/ Action for Stroke, to Slovakian by our member organisation Porazka.sk, the Croatian Stroke Society, with many other translations to come in the next couple of months.

Jan 11, 2019
Article written by Francesca Fedeli, Founder of Fightthestroke.org, advocating for young stroke and CP survivors
Fightthestroke has been selected among 65 practices and 11 policies from around the world that help persons with disabilities on the Zero Project Award 2019, celebrating this year the topic of Independent Living and Political Participation. Project Mirrorable indeed has been awarded as a unique platform that improves the Motor Function in Young People with Cerebral Palsy.
 Fightthestroke, an Italian social enterprise founded in 2014, has developed an online platform called ‘Mirrorable’ to support rehabilitation of young stroke survivors. Mirrorable is a home-based therapy programme based on Action Observation Treatment, which states that by observing and imitating the actions of others we trigger specific neurons (‘mirror neurons’) in our own brain. Young stroke survivors are paired through AI and via a video platform and undertake tasks together to improve motor skills. A clinical trial on children with unilateral cerebral palsy has demonstrated an improvement in hand motor function compared to traditional rehabilitation, along with high levels of adherence and engagement.
Fightthestroke, an Italian social enterprise founded in 2014, has developed an online platform called ‘Mirrorable’ to support rehabilitation of young stroke survivors. Mirrorable is a home-based therapy programme based on Action Observation Treatment, which states that by observing and imitating the actions of others we trigger specific neurons (‘mirror neurons’) in our own brain. Young stroke survivors are paired through AI and via a video platform and undertake tasks together to improve motor skills. A clinical trial on children with unilateral cerebral palsy has demonstrated an improvement in hand motor function compared to traditional rehabilitation, along with high levels of adherence and engagement.
“MaVi discovered herself for the first time, when practicing with Mirrorable in front of the TV screen. The project for me was “moving”, it touches the heart and, if there is a mirror heart, it touches it too!”
– Valentina, mother of MaVi, who took part in the Mirrorable pilot
Problems Targeted
There are few effective and accessible evidence-based solutions to help rehabilitate motor skills in the estimated 17 million children with cerebral palsy worldwide.
Solution, Innovation, and Impact
The Mirrorable platform uses the scenario of learning to become a magician to encourage young stroke survivors to practice motor skills every day for a month. Children in the Mirrorable’s clinical trial received a toolkit with a computer, a 3D camera, and selection of booklets and magic tricks. They used these to imitate the magician in videos on a cloud-based platform. They were also matched with peers via video link to practice together and learn from each other. The IT-platform uses an algorithm to ensure the best possible match in terms of motor skills, cognitive abilities, etc. to support reciprocal teaching and rehabilitation. The gaming approach of Mirrorable increases the appeal for children and encourages them to practice. In the market version, the 3D camera has been replaced by artificial intelligence technology which tracks and records the child’s movements and emotions so that progress can be measured by the child, family members, and health professionals. Results of a clinical trial, presented in 2018, showed a 26 per cent improvement in motor function, increased family engagement, and 100 per cent adherence to the daily exercises.
Funding, Outlook, and Transferability
Support developing Mirrorable and the clinical trial came from corporate fundraising, grants and private donors, but the project was especially driven by the Fightthestroke co-founders Francesca Fedeli and Roberto D’Angelo who experienced themselves a young stroke survivor in their family. Following the trial Mirrorable is now developing a business model to bring the product to a wider market, while keeping prices as low as possible for families of young stroke survivors.
Mirrorable’s cloud-based technology makes easily transferable, and the operating system is already available in Italian, Spanish and English. Fightthestroke is exploring whether the programme might be appropriate for other target groups, such as adult stroke survivors or people with Parkinson’s disease. Fightthestroke has also developed an offline programme to complement Mirrorable’s online platform, and held its first intensive Mirrorable sports camp, including Habit and AOT treatments, for children with unilateral cerebral palsy in August 2018.
About the Practice at a Glance
NAME OF INNOVATIVE PRACTICE: Mirrorable
ORGANIZATION: Fightthestroke
COUNTRY OF IMPLEMENTATION: Italy
 Facts and Figures
Facts and Figures
– A recent clinical trial demonstrated that Mirrorable online users realized a 26 per cent improvement in motor function.
– The Mirrorable model costs approximately half as much as conventional therapy.
– The Mirrorable ecosystem can be easily replicable for other target groups, as adults who suffered a brain stroke.
 Contact
Contact
Francesca Fedeli
francesca@fightthestroke.org
Fightthestroke Website
Links and Further Reading:
Mirrorable website
Mirrorable founders’ Ted Talk (video)
Mirrorable demo video

Jan 4, 2019
First published on ScienceDaily.com
In a medical records analysis of information gathered on more than 6,000 people, Johns Hopkins Medicine researchers conclude that simply asking older adult patients about their weight history at ages 20 and 40 could provide real value to clinicians in their efforts to predict patients’ future risk of heart failure, heart attacks or strokes.
In a report published Nov. 14 in the Journal of the American Heart Association, the investigators say the younger-weight question is potentially a cost-efficient, high-value “ask” likely to help physicians decide how to advise and treat their older patients, particularly now that many people change primary care physicians throughout their lives, and lifelong health records may not transfer. Asking this simple question about prior lifetime weights provided prognostic information about a person’s heart failure risk that was incremental to their measured weights at older ages and other measured traditional heart disease risk factors.
“We’ve known that the longer a person is obese, the more it becomes problematic by increasing their heart failure risk,” says Erin Michos, M.D., M.H.S., associate professor of medicine at the Johns Hopkins University School of Medicine. “That is why measuring a person’s weight at older ages may not tell the whole story about their risk. There’s now more evidence that newly obese people are in overall less danger. Our findings emphasize the importance of lifelong maintenance of a healthy weight, as greater cumulative weight from young adulthood is more risky to heart health.”
“We already routinely measure weights during a patient’s clinic visit to make health recommendations, but we think adding this low-tech question about their prior weight histories can further help direct clinical care,” she adds. “While we acknowledge that self-reported weight history is imperfect, at the very least, asking the question sparks patient reflection and self-motivation to get back to healthier weights from their younger ages.”
Heart attacks, strokes and other cardiovascular diseases remain the No. 1 killers of Americans. Heart failure, also known as congestive heart failure, is a condition marked by a gradual weakening and stiffening of the heart muscle, diminishing its ability to pump blood. Physicians routinely attempt to assess risks for heart disease and heart failure as patients age with measures of blood pressure, cholesterol, exercise levels, family history, diet and weight, Michos noted. Although a single weight measurement in an older adult is helpful, she says, weight history is even more informative, and the new study was in part designed to identify a practical way of getting it that would be considered informative enough to add to clinical care.
For the study, the researchers used data already gathered on 6,437 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) recruited between 2000 and 2002 who were age 45 to 84 at time of enrollment into the study. Participants were followed an average of 13 years, and lived in six U.S. communities: Baltimore, Maryland; Chicago, Illinois; Forsyth County, North Carolina; New York City, New York; Los Angeles County, California; and St. Paul, Minnesota. On average, they were 62 years old at the study’s start. Almost 53 percent of the participants were women. About 39 percent of participants were white, more than 26 percent were African-American, 22 percent were Hispanic and a little more than 12 percent were Chinese-American.
Each participant filled out a survey that reported their weight history at age 20 and 40. Their weights were further tracked during the study period using measurements from a standardized scale over five different in-person visits. All weights were converted to body mass indexes (BMI) by dividing the weight by the square of height. A BMI less than 25 kilograms per meter squared was considered normal, while a BMI between 25 and 30 was considered overweight, and 30 and above was considered obese.
By the end of all participants’ last visit, 290 people had experienced heart failure, and 828 experienced cardiovascular disease events such as heart attacks, stroke and or death as determined by participant and family interviews and patient medical records.
As expected, Michos says, the standard measured weights taken at clinic visits during the 13-year study period were associated with later heart failure risk, with a 34 percent increased likelihood of heart failure for every 5 kilograms per meters squared increase in BMI, after accounting for other established heart disease risk factors such as age, smoking, physical activity, blood pressure and diabetes. But then her team found that even after taking into account these current measured weights at older ages, that having a self-reported history of obesity at age 20 (144 participants) was associated with a more than threefold risk of heart failure, and having a history of being obese at age 40 (716 participants) doubled the risk compared with people who had a BMI in the normal range at those ages.
“Our study confirms that maintaining a normal weight over the lifespan is the most ideal, and that when and for how long a person becomes obese are highly informative in assessing heart disease risk in older adults,” says Michos.
Michos cautioned that the new study was designed to look at associations between self-reported lifetime weights and heart disease risk over time, and not determine cause and effect or attempt to determine the accuracy of patients’ recall of their weight at young ages. Patient self-reporting can result in bias or imperfect memory, but the researchers believe most older adults have reasonably accurate recall of their younger adult weight. Their study findings suggest that even with these known limitations of weight recall, that simply asking about weight history was helpful in risk assessment. Right now, clinicians just don’t routinely ask about a person’s weights at key life points such as young- and mid-adulthood, Michos says, but it is so easy to do.
Michos says that we need to investigate how we can incorporate this ask (about lifetime weight recall) into electronic health records and into clinical practice.
About 1 in 3 deaths in the U.S. are due to heart disease, according to the American Heart Association. About 92 million American adults are living with some form of cardiovascular disease. About 5.7 million people in the U.S. live with heart failure, and more than half a million are diagnosed each year. More than half of people with heart failure will die within five years of diagnosis, according to the Centers for Disease Control and Prevention.
Story Source:
Johns Hopkins Medicine. “Your weight history may predict your heart failure risk: Low-tech reporting on earlier weights may guide clinical care.” ScienceDaily. ScienceDaily, 12 December 2018. <www.sciencedaily.com/releases/2018/12/181212093327.htm>.

Dec 28, 2018
Another exciting issue of European Neurological Review is now released, highlighting new advances in the field of Neurology, as well as featuring SAFE’s information about the Stroke Action Plan for Europe.
 We find one of the case reports from this issue particularly interesting, covering a rare syndrome that can occur in persons with an ischaemic stroke.
We find one of the case reports from this issue particularly interesting, covering a rare syndrome that can occur in persons with an ischaemic stroke.
Charles Bonnet syndrome (CBS) is characterised by the presence of visual hallucinations (VH) and visual sensory deprivation in individuals with preserved cognitive status and without a history of psychiatric illness. CBS is a rare, underdiagnosed and under-recognised syndrome, which was first described in 1769 by Charles Bonnet, who observed this phenomenon in his grandfather.
The prevalence of CBS is not consistent between authors. Some studies have stated that 0.47% of the general population suffer from CBS – this number can increase to around 15–30% when referring to patients with visual impairment. The disparity in CBS prevalence can be explained by the absence of clear diagnostic criteria, the necessity of different specialties to recognise or exclude other disorders and the incapability of patients to express the symptoms.2,3 CBS usually occurs in elderly people with compromised visual function and can be a rare manifestation of an injured visual pathway. Secondary lesions to multiple sclerosis, ischaemic stroke, temporal arteritis and meningiomas can explain the syndrome. This case report presents a variant of CBS as consequence of an ischaemic stroke in left occipitotemporal regions. In our view, the particularities and variations of CBS should be widespread, as it can be the only manifestation of an ischaemic stroke that requires appropriate and immediate management.
You can read the full case report here and you can find more articles from the latest issue here.
Dec 21, 2018
Oruen – The CNS Journal has now been published online. In this issue you can find the SAFE special report on stroke prevention project and Stroke Action Plan for Europe advert. SAFE is also mentioned in the two ANGELS articles.
The current issue also brings you the following reviewed articles:
Clinical Outcomes and Work Flow Optimisation with Pipeline System and Shield Technology (Istvan Szikora, Saleh Lamin, Mohamed Aggour)
Innovations in Endovascular Treatment of Acute Ischemic Stroke and Cerebral Aneurysms (Hannes A. Deutschmann, Marc Ribo, Mathieu Sanchez)
The ANGELS Initiative: More and better Stroke-ready Hospitals across the globe (Rob Goodwin)
Improving stroke care across the world: The Angels Initiative (Valeria Caso, Magd Fouad Zakaria, Ales Tomek, Robert Mikulik, Sheila Cristina Ouriques Martins, Thang Huy Nguyen, Anastasia Rossouw)
Stroke Prevention in atrial Fibrillation: update with NOAC Treatment and the impact of Reversal (Dr. Allison Kirsop)
Transition of ADHD Patients from Childhood into Adulthood (Dr Allison Kirsop)
An Introduction to the Internal Capsule in Schizophrenia (Dr. Matthew Williams)
About Oruen – The CNS Journal
The journal is owned and published bi-annually by Oruen Limited; it is a peer-reviewed, open access publication, and has received CME accreditation from the European Accreditation Committee in CNS (EACIC) with a 100% focus on original CNS research topics, and the latest advances, diagnoses, and treatment of CNS disorders. Oruen – The CNS Journal is distributed in print and electronically to thousands of physicians, researchers, academics, nurses, and related healthcare professionals with an interest in CNS disorders. Both subscription and access are free and there are no contributory author fees for publication. Papers submitted for publication are accepted based on their originality, likely impact on and relevance to clinical practice, data quality, and overall potential interest to the journal’s readership.

Dec 20, 2018

Dec 14, 2018
First published on ScienceDaily.com
Aggressive treatment of hypertension in stroke patients could do more harm than good in the long term, according to a new study from researchers at the University of Georgia.
Sixty percent of stroke patients admitted to U.S. emergency rooms have elevated blood pressure, and many studies say that having high blood pressure at the time of stroke can lead to higher rates of death and major disability.
But lowering blood pressure too much with medications may actually be working against the body’s protective response to maintain blood flow into the affected brain tissues.
“This presents a clinical dilemma,” said study author Changwei Li, an assistant professor of epidemiology and biostatistics at UGA’s College of Public Health.
It may be better to keep blood pressure a little higher than normal, closer to 140/90 mmHg rather than a “good” blood pressure of 120/80 mmHg, but that leaves the question of best practices a little open-ended.
“Currently, hypertension treatment for acute stroke patients is based on physicians’ clinical experience and judgement,” said Li. “There is no guideline on how low the blood pressure should be maintained.”
The key is to find the right balance between maintaining blood flow to the brain and reducing negative short- and long-term effects.
To help identify this optimal blood pressure, Li and his co-authors looked at the relationship between blood pressure during stroke and both short- and long-term health outcomes for over 4,000 Chinese stroke patients participating in the China Antihypertensive Trial in Acute Ischemic Stroke study. One group of stroke patients received extensive treatment for high blood pressure while a control group received no treatment at the time of their stroke.
Li and his collaborators tracked blood pressure changes over time in both the treatment and control groups during the first week of hospital admission and compared patient health at one week, three months, one year and two years following the stroke across patients of different blood pressure trajectories.
To access the full article, please click here.
Story Source:University of Georgia. “Optimal blood pressure treatment for stroke patients.” ScienceDaily. ScienceDaily, 10 December 2018. <www.sciencedaily.com/releases/2018/12/181210142059.htm>.

Dec 8, 2018
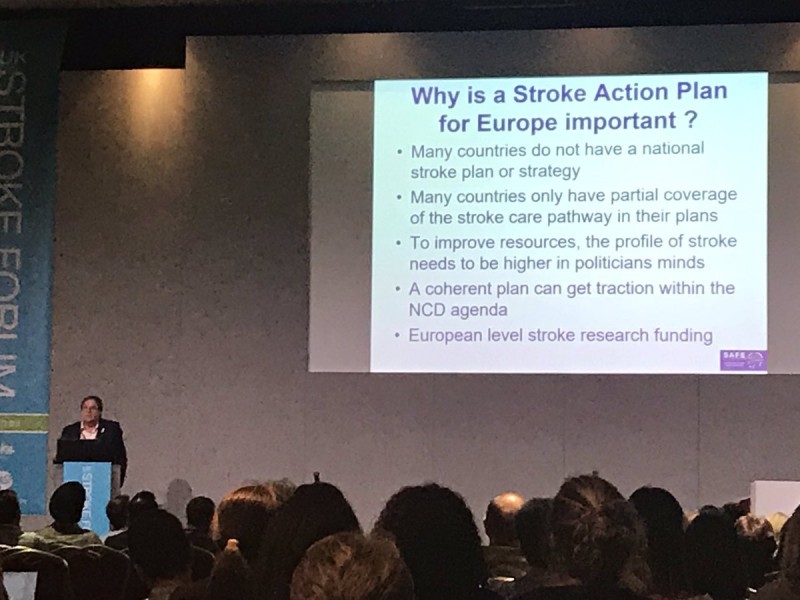
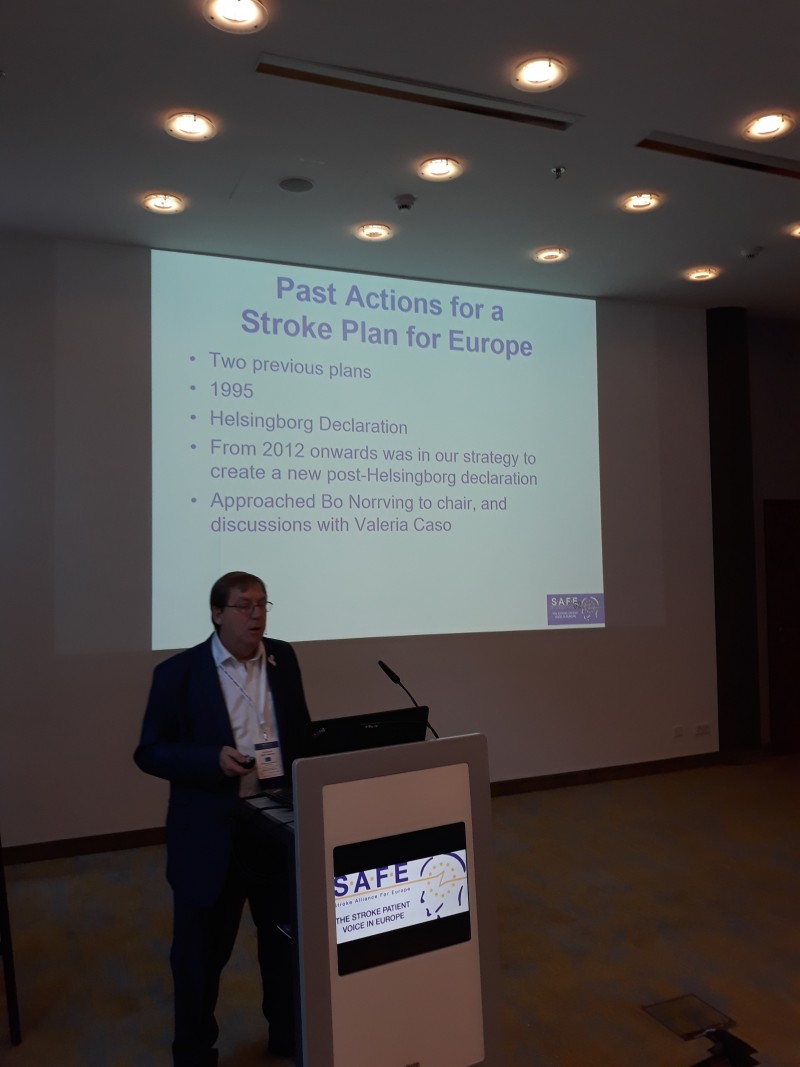
Jon Barrick, SAFE President, presented Stroke ACtion Plan for Europe 2018-2030 at the 13th UK Stroke Forum Conference (#UKSF18). The #UKSF18 took place at The International Centre, Telford,UK, from 4 – 6 December 2018.
“There was a great need for a document such as the Stroke Action Plan for Europe. Many European countries do not have a national stroke plan or strategy and many of them only have partial coverage of the stroke care pathway in their plans” said Barrick.
This 3 day multidisciplinary conference brought together over 110 expert speakers and researchers, all committed to improving stroke care.
About UK Stroke Forum
The UK Stroke Forum is a coalition of over 30 organisations all committed to improving stroke care in the UK. The coalition is underwritten by the Stroke Association UK.
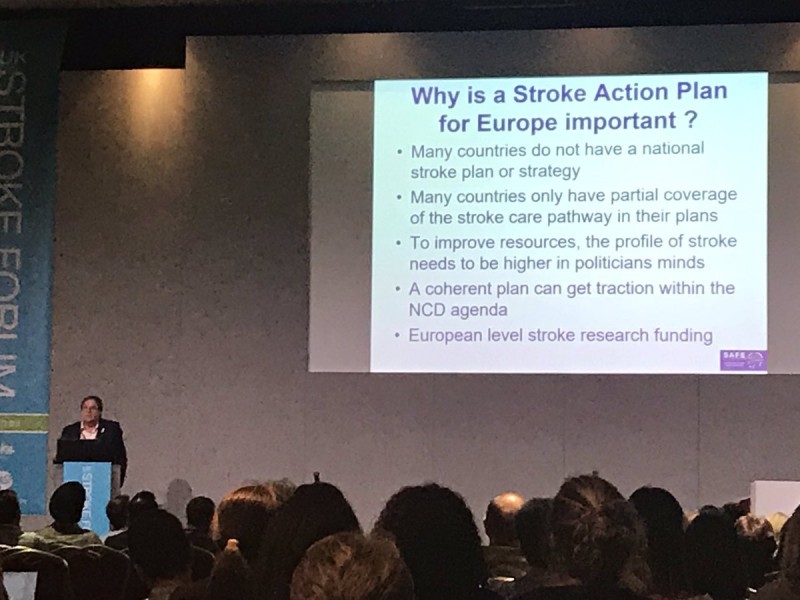
Photo by Sarah Belson

Dec 4, 2018
Roman Shwed from Ukraine is a stroke survivor and a first-time attendee at SAFE Working Conference in Berlin. He shared with us his unique view of this event, kindly agreeing that we share it further with the world. We at SAFE believe you will enjoy it… (In the photo above, Roman Shwed is the first person on the left).
A “TOUNGUE IN CHEEK”, SHORT REPORT ‘SO TO SPEAK’, OF MY WONDERFUL EXPERIENCES IN THE CITY OF BERLIN, GERMANY, NOT TO BE CONFUSED WITH BERLIN, NEW JERSEY, OR ANY OTHER BERLIN ON THE PLANET…
…anyway,
I’m talking about our “SAFE 2018 WORKING CONFERENCE”, which was masterfully dreamed up, programmed, and prepared, by Jon Barrick, the Prez., his VP Markus Wagner, plus Secretary Monique Lindhout, Treasurer Grethe Lunde, Board Members Ivan Milojevic’, Anita Arsovska, Pnina Rosensweig, Kolbrun Stefansdottir, and on the 27th through 30th November, professionally executed by the staff which included Sandra Jackson, Lucinda Shaw, Gary Randall, Jelena Misita, and Victoria Brewer. If I missed anyone, or misspelled a name, kindly forgive my mistakes…this was the very first, never ever before attended, SAFE Working Conference in my whole life, and I meticulously copied all that info from the SAFE Annual Report…so there !
…but I digress,
If anyone has any doubts about my feelings about this conference, let me tell you, I was duly impressed, wow-ed, amazed, and, …in a word, the conference “knocked my socks off” ! I learned a bunch of new stuff about “Life after Stroke”, and reflected on my own situation. What kind of Stroke did I experience ? After seeing all the Delegates, especially other Stroke survivors, and remembering what the 3 types of Stroke are, namely: Ischemic, Hemorrhagic, and TIA, my opinion about my Stroke changed dramatically.
Now when friends on the street will ask me, “Roman, why do you walk so funny ?”, I’d explain that “Moi had a Stroke”…then they usually asked me, politely, “oh?… what kind of Stroke was it ?”, showing off their assumed Stroke knowledge. I used to be very exact in my replies, telling them that it was an Ischemic Stroke, and then, the questioner would, invariably, nod his or her head, sympathetically. Well, this routine is changing, and from now, when asked, I will tell them, “I had STROKE LIGHT ”, for which they’ll have no smarty pants reply, and also this will, hopefully, generate no additional questions. I did, for a while, consider calling mine the Diet Coke way, like “DIET STROKE”, but it just wasn’t sexy enough.
…but, again, I digress,
My friend Dr.Dmytro Gulyayev, (my Ukrainian co-conspirator), who took care of my Stroke recovering body, introduced me to Sandra, and we immediately became friends, but then small wonder, everyone else who was there accepted me and my ‘Drunken Sailor’ walk without question. It’s really comforting to be among people that understand what you went through, and are still, like you, overcoming this health burp in their life. The Conference was peopled by Delegates from “almost” all European Countries, but everyone spoke English…well, let me clarify. There is the Queen’s English, as spoken by Jon, Sandra, and a few others, then there was some Brogue English, as spoken by my Irish & Northern Irish friends, a little North American English, like mine, and the rest spoke European, or as I fondly refer to, YODA English. Yoda would be very proud of us all, because every single Delegate is battling the DARK STROKE Force like a true Jedi Knight !
…but I can’t help myself…I still digress,
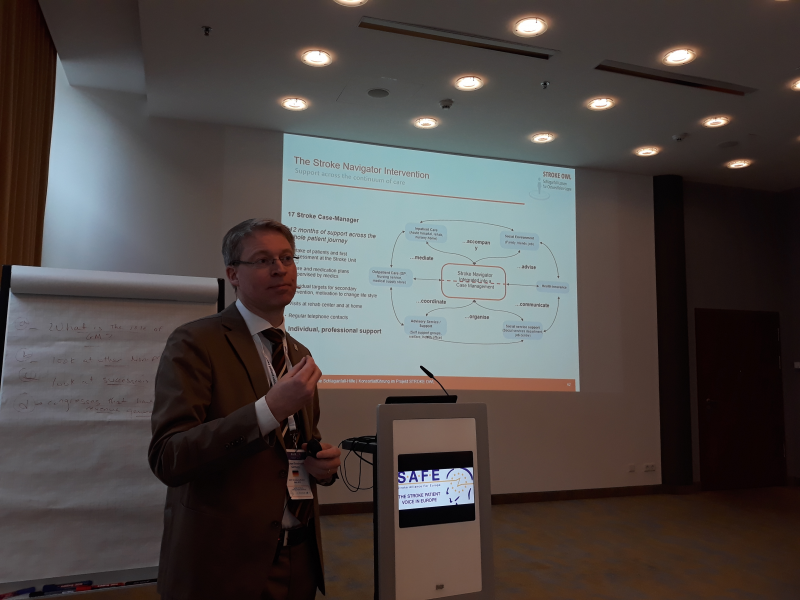
As the second day came into play, Integrated Care in Germany was presented by Markus Wagner, our V.P., and then Michael Brinkmieir, the Chairman of the German Stroke Foundation, had a very good presentation of Case & Care Management in East Westphalia. Our table started to speculate…”if there is a Westphalia, there must be an Eastphalia, and therefore – a West Eastphalia”…but we never reached a final agreement, so if you have any doubts, just GOOGLE it. Anyway, the Workshops were great, and very useful, especially to a “nebish” like me. Dmytro and I were there to Listen & Learn, and our East Cluster Workshop, which was in Hamburg…the Room, not the Burg, explained our moderator, and allayed our fears of having to travel to another City.
If I have any complaints, it’s about the food. The meals were great, tasty, and I think that I must have gained a kilo or two. It just isn’t fair to guy’s like me, when you place such tasty temptations before us. The Wednesday Night Feast at Maximillian’s was superb, and I’m sure that our ladies enjoyed the waiters in “Lederhosen”. I believe that everyone, Staff and Jedi Knight, had 2 pretzels each, but who cares as long as no one broke into song or yodelling.
ALL THAT’S LEFT TO SAY IS A GREAT BIG THANK YOU TO THE LEADERSHIP & STAFF OF SAFE, AND OUR WONDERFUL SPONSORS … “THANK YOU” IS CERTAINLY AN UNDERSTATEMENT…BECAUSE MY VOCABULARY IS TOO LIMITED TO DO JUSTICE TO THE BERLIN CONFERENCE,
AND I MUST ADD A HEARTFELT – “YO, AND A FIST BUMP”, THANK YOU DELEGATES – JEDI KNIGHTS ALL … MAY THE “SAFE” FORCE BE WITH YOU !
I DID MEET SOME OF YOU PERSONALLY, AND LOOK FORWARD TO MEETING THE REST OF YOU REAL SOON !
SMILINGLY YOURS,
Roman “Toungue in Cheek” Shwed,
UKRAINE

Dec 2, 2018
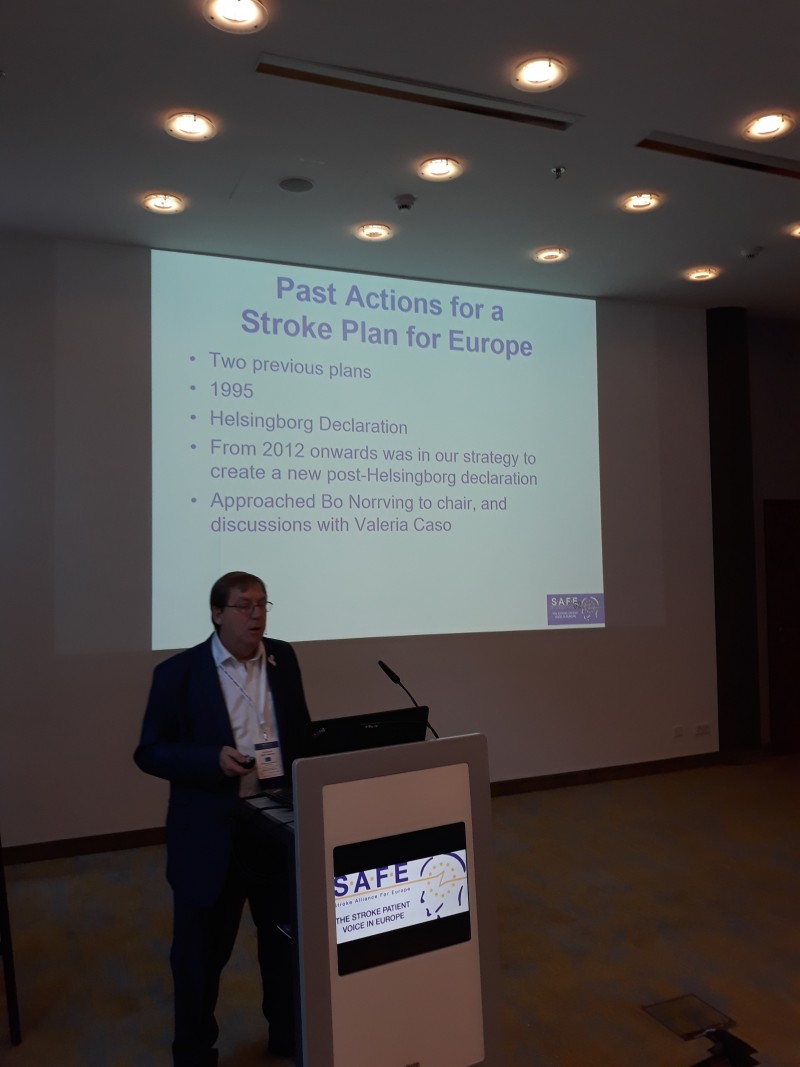
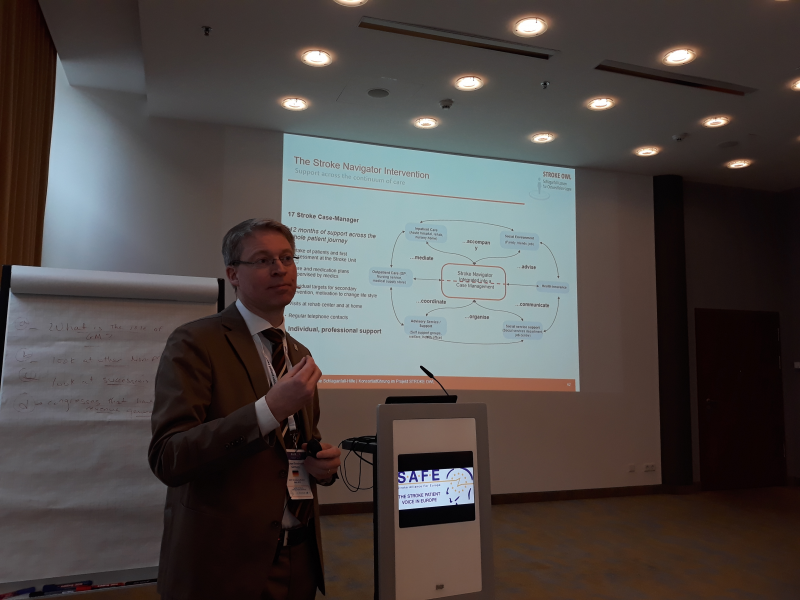
SAFE held this year’s Working Conference and the General Assembly in Berlin, Germany. The event was very well attended, with over 100 delegates and representatives of SAFE’s industry partners.
The hosting organisation was the Stiftung Deutsche Schlaganfall Hilfe, SAFE’s member organisation from Germany, whose President, Michael Brinkmeier presented their latest projects to the auditorium. SAFE President Jon Barrick and ESO Board member Heinrich Audebert gave presentations on how the Stroke Action Plan for Europe 2018-2030 was created, including the overarching recommendations on the seven domains, from Primary Prevention to Life After Stroke.
The working conference was dedicated to updating our members on the current projects and presenting plans for the next period, until 2020 and beyond.
Stroke Support Organisation Faculty Tool was completed just before the SAFE’s annual gathering and SSOFT Project Director, Victoria Brewer gave a wrap up, summarizing the achievements and giving recommendations for future use and increased engagement.
You can access the complete Working Conference Agenda here.
On Friday, 30th November, SAFE had a General Assembly. Three new Board members were elected: Grethe Lunde from Norway (Norsk forening for slagrammede (NFS)) as a North Cluster Representative, Chris Macey from Ireland (Irish Heart Foundation) as Treasurer and Marina Charalambous from Cyprus (Cyprus Stroke Organisation) as Board Member at Large.

Two new organisations were ratified and became full SAFE members: Porážka.sk from Slovakia and CEREBRUM from Czech Republic.
SAFE awarded stroke support organisations from the following countries: Turkey, Spain, Serbia,Croatia, Portugal, Iceland and Cyprus for their work in fighting stroke, supporting survivors and their families and building the patient voice during 2018.

In addition, SAFE Annual Report and Strategy were discussed, as well as the upcoming SAFE political activities at EU level.







 Fightthestroke, an Italian social enterprise founded in 2014, has developed an online platform called ‘Mirrorable’ to support rehabilitation of young stroke survivors. Mirrorable is a home-based therapy programme based on Action Observation Treatment, which states that by observing and imitating the actions of others we trigger specific neurons (‘mirror neurons’) in our own brain. Young stroke survivors are paired through AI and via a video platform and undertake tasks together to improve motor skills. A clinical trial on children with unilateral cerebral palsy has demonstrated an improvement in hand motor function compared to traditional rehabilitation, along with high levels of adherence and engagement.
Fightthestroke, an Italian social enterprise founded in 2014, has developed an online platform called ‘Mirrorable’ to support rehabilitation of young stroke survivors. Mirrorable is a home-based therapy programme based on Action Observation Treatment, which states that by observing and imitating the actions of others we trigger specific neurons (‘mirror neurons’) in our own brain. Young stroke survivors are paired through AI and via a video platform and undertake tasks together to improve motor skills. A clinical trial on children with unilateral cerebral palsy has demonstrated an improvement in hand motor function compared to traditional rehabilitation, along with high levels of adherence and engagement. Facts and Figures
Facts and Figures Contact
Contact

 We find one of the case reports from this issue particularly interesting, covering a rare syndrome that can occur in persons with an ischaemic stroke.
We find one of the case reports from this issue particularly interesting, covering a rare syndrome that can occur in persons with an ischaemic stroke.