Mar 15, 2019
This text was was first published on www.svds-at-target.eu
In November 2018 the Zoom@SVDs study included the 60th participant, thereby reaching its milestone for midterm recruitment. The Zoom@SVDs study is an observational study that aims to advance our understanding of Small Vessel Disease, a condition in which the small blood vessels in the brain are damaged. We do this by zooming in on the small vessels with one of the strongest MRI scanners currently available for humans, located in the UMC Utrecht.
This study builds on a collaboration between the LMU in Munich (Germany) and the UMC Utrecht (Netherlands). In order to undergo a scan in the strong MRI in Utrecht, the 28 participants that were recruited so far in Munich travelled from all over Germany to Utrecht for an additional visit. Of course, the logistics of this study are very challenging, because flight tickets, train tickets and hotels have to be arranged as well. Also, all study information needed to be officially translated from Dutch to German and the researchers in Utrecht had to refresh their German language skills. However, these joined efforts have resulted in fast recruitment with happy participants and high-quality data.
Analyses of the first patient data have just started, of which we aim to publish the first results in the coming year. Of course, we will continue our recruitment and will continue to work in close collaboration. This study builds on our dedicated participants and good teamwork; thanks to all involved!
Mar 12, 2019
First published on ScienceDaily.com
Tumult in the bacterial community that occupies your gut — known as your microbiome — doesn’t just cause indigestion. For people recovering from a stroke, it may influence how they get better.
A recent study by Allison Brichacek and Candice Brown, researchers in the West Virginia University School of Medicine, suggests that stroke patients’ microbiomes — and even the structure of their guts — may still be out of kilter a month after the stroke has passed.
“We’re interested in the gut-brain axis — how the gut influences the brain and vice versa,” said Brichacek, a doctoral student in the immunology and microbial pathogenesis graduate program. She presented her findings at the International Stroke Conference in February.
Previous studies indicated the immediate effects a stroke can have on someone’s microbiome, but they didn’t explore whether these effects lingered. To find out, Brichacek, Brown and their colleagues — including Sophia Kenney, an undergraduate majoring in immunology and medical microbiology, and Stan Benkovic, a researcher in Brown’s lab — induced a stroke in animal models. Other models — the control group — didn’t have a stroke. The researchers compared the two groups’ microbiomes three days, 14 days and 28 days post-stroke. They also scrutinized their intestines for microscopic disparities.
Bacterial friend or foe?
One of the researchers’ discoveries was that a certain family of bacteria — Bifidobacteriaceae — was less prominent in post-stroke models than in healthy ones both 14 and 28 days out. If the name of the family sounds familiar, that’s probably because Bifidobacterium — a genus within the Bifidobacteriaceae family — is a common ingredient in yogurt and probiotics. These bacteria are known for supporting digestive health and may be associated with better outcomes in stroke patients.
Read the full article here.

Mar 11, 2019
Sharing #LifeGoals has become a popular trend on social media. A campaign from the European Federation of Neurological Associations [EFNA] and supported by many organisations across Europe will put a new spin on the trend by instead seeing patient advocates and supporters share their #BrainLifeGoals.
The #BrainLifeGoals campaign will raise awareness of the impact of neurological diseases by exploring the dreams and aspirations of those living with a brain disorder.
You can find out more about the campaign at www.efna.net/brainlifegoals and by following the #BrainLifeGoals hashtag on social media.

Mar 7, 2019
The German Stroke foundation started its work in January 1993. To celebrate the anniversary the foundation launched a new campaign: “I set a sign.” A newly designed website went online in October and the Integrated Care Project “STROKE OWL” enrolled the first patients.
Author: Ina Armbruster
 “I set a sign.”
“I set a sign.”
A red stripe above the eyebrow represents the stroke. A sign that celebrities, stroke victims and supporters set to raise awareness and show their solidarity towards stroke-victims. The campaign “I set a sign” was launched in May 2018 at the “Rosenball”, a significant charity event for the German Stroke Foundation in Berlin. During this event many guests had their picture taken with a red stripe above their eyebrow and uploaded their “sign” on social media or the campaign-page www.schlaganfall.de.
The campaign was running on many different channels. The local billboard company supported the foundation by offering rent-free billboards for a couple of weeks which were set up all over Gütersloh, the hometown of the foundation. Thanks to the cooperation with the TV channels of the RTL Group more than 100 million viewers have seen the TV-spot “I set a sign” so far. The advertisement has been published in many magazines with an edition of 1,5 million in total. People who have set a sign were portrayed with their individual stories on facebook once a week. Up to a couple of hundred users liked or commented on these posts.
The foundation used the campaign to raise awareness of stroke – because everyone can have a stroke, regardless of age, gender or social background.
New website
 The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters.
The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters.
Additionally, the website is now accessible for mobile devices as well. In 2019 the website will be updated with more information. The foundation also plans to add further technical features. www.schlaganfall-hilfe.de
Project “STROKE OWL”
 The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke.
The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke.
About the project:
- A specialised stroke case manager gets in touch with the patient at the stroke unit. The patient can take part in the program if he or she fulfils certain enrolement criteria. The case manager visits the patient during rehab and at home.
- All case managers have experience with stroke patients. Most of them are nurses or therapists with further education in case management.
- The case manager informs patients and their families about everything they need to know after having a stroke and gives them advise and support. The manager organises the treatment, helps filling out applications, and looks after the patient in general.
- The manager supports the patient for one year. The foundation´s goal is to enrol 2000 patients in the program.
By proving the advantages of a case management not only for the patients but also for the health care system in general the German Stroke foundation wants to support the establishment of stroke case management, which in the end is payed by the insurance companies.
Looking forward to 2019
 The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning:
The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning:
– seminar for parents of children who had a stroke
– implementing a second case manager in Germany for children who had a stroke and their families
– continuing the project “STROKE OWL”
– raising attention to the topic with a campaign for the “Day against stroke” in May (with a focus on “The invisible consequences of stroke”, e.g. concentration-problems, emotional imbalance or neglect)
– 4-day workshop for young stroke patients between 18 and 50
and much more…

Feb 27, 2019
This news first appeared in the WSO Newsletter
The World Stroke Organization is proud to share its most recent and much expected publication: the Global Stroke Fact Sheet.
The 10-page document overviews the best available scientific evidence to provide reliable and up to date data on stroke and its impact around the world. Using reliable and consistent stroke data to support stroke advocacy helps to build awareness of the scale of the disease and supports the call for urgent action at global, regional and national levels.
The values in the document have all been extracted from the most current Global Burden of Disease Stroke Statistics Worldwide for the year 2016. The present document and all its subsequent revisions are reviewed and approved by the WSO leadership.
We hope that Global Stroke Fact Sheet will be a valuable resource and a useful point of reference in your work, practice, and research.
We invite you to share the document with your colleagues, students and partners. Thank you for your continuous support for the work of WSO.
You can access and download the Global Stroke Fact Sheet here
For more information please visit WSO website.

Feb 20, 2019

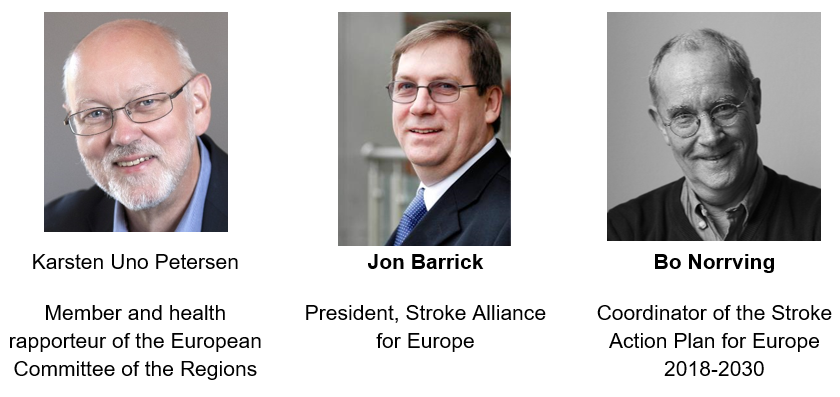
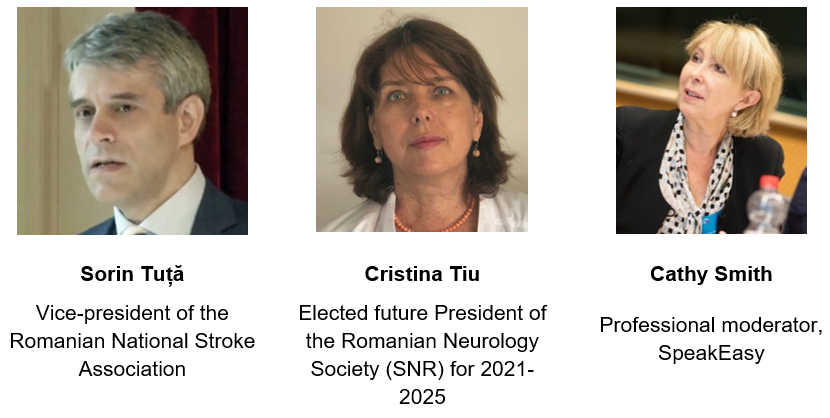
The Stroke Alliance for Europe (SAFE) invites you to attend the event ‘Joining forces to prevent and control non-communicable diseases: The role of policy in tackling stroke’, under the patronage of the Romanian Presidency of the Council of the European Union (#RO2019EU), which will take place on 28 March 2019, in Brussels, at the European Committee of the Regions. The event will be organised by SAFE in collaboration with the European Stroke Organisation and the Romanian National Stroke Association.
The event will look into the role of policy and policy stakeholders in combating stroke-related challenges and addressing the burden of stroke, as well as in achieving the ambitious targets of the ‘Stroke Action Plan for Europe 2018-2030’. The discussions will be integrated into the expected health priorities for the Romanian and upcoming Finnish and Croatian presidencies as well as current and future EU action for preventing and controlling non-communicable diseases.
The Action Plan focuses on seven key domains, namely primary prevention, organisation of stroke services, management of acute stroke, secondary prevention, rehabilitation, evaluation of quality and outcomes as well as life after stroke. It outlines four overarching targets to be achieved by all European countries and health systems by 2030, which are complemented by further specific targets set for each of the seven domains. SAFE and ESO are currently pursuing its dissemination and implementation at national, regional and local levels.
With an expected 35% increase in the incidence of stroke in Europe by 2035, as highlighted in the Burden of Stroke in Europe Report, this conference represents an important opportunity to bring together European, national and local policy-makers and other key stakeholders to address the disparities across the stroke care pathway between and within European countries.
REGISTRATIONS
Registrations for our event are now open! If you are interested in joining us on 28 March at the CoR please register here. On the other hand, if you cannot come to Brussels but would like to follow the live streaming of the event, you can show your interest here.
PROGRAMME
The event programme will be published soon.
THE SPEAKERS

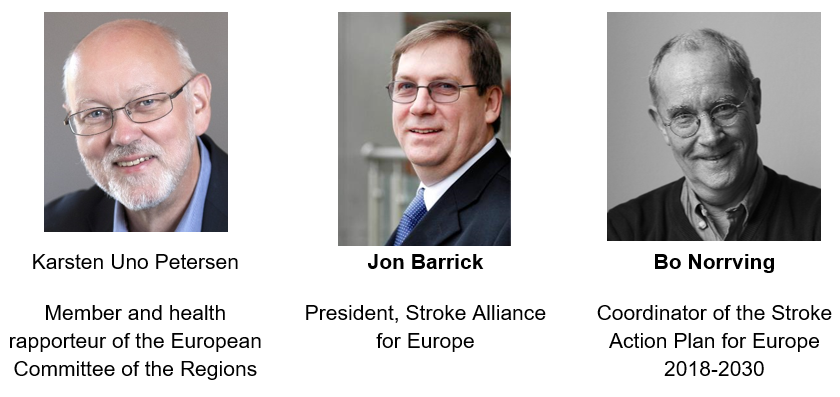
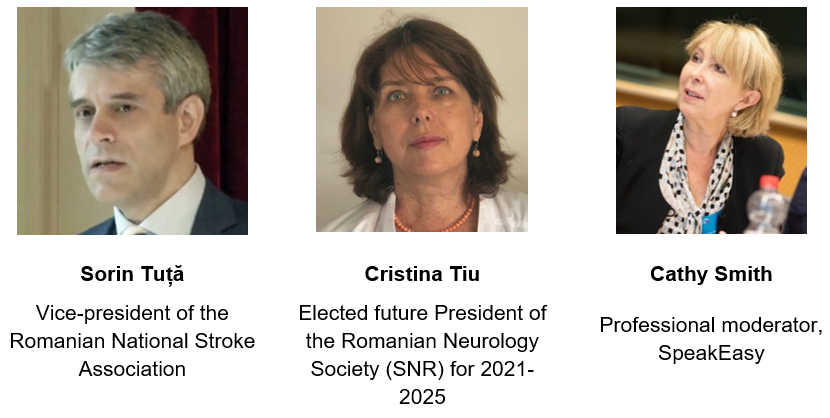
To view more information on the speakers click here.
ORGANISERS
The event will be organised by SAFE in collaboration with the European Stroke Organisation (ESO) and the Romanian National Stroke Association (ANRS).

About SAFE
SAFE is an umbrella organisation that represents a range of stroke patient organisations across Europe that were affected by stroke. SAFE’s vision is to work towards reducing the number of strokes in Europe as well as ensuring that everyone who is affected by stroke gets the help and support they need.
By combining the resources of patient organisations across Europe SAFE is working for better stroke prevention, more effective stroke care, greater public awareness and increased research activity within Europe.
About ESO
ESO is a pan-European society of stroke researchers and physicians, national and regional stroke societies and lay organisations. The aim of the ESO is to reduce burden of stroke by changing the way that stroke is viewed and treated. ESO serves as the voice of stroke in Europe, harmonising stroke management across the whole of Europe and taking action to reduce the burden of stroke regionally and globally.
About ANRS
ANRS is an independent, not-for-profit, non-governmental and apolitical Romanian association of physicians with scientific, medical and social goals regarding stroke prevention and management optimisation in accordance with the European and WHO standards. The association organises congresses, conferences, round tables, practical demonstrations and symposia that seek to promote up-to-date stroke education, according to the latest scientific research and validated therapeutic progress.
ENDORSEMENTS
The event will be held under the patronage of the Romanian Presidency of the Council of the European Union and hosted at the European Committee of the Regions (CoR).

About the Romanian Presidency of the Council of the European Union
Romania will hold the Presidency of the Council of the EU from January to June 2019. The Council of the European Union is the institution where the governments of the EU Member States defend their own country’s national interests in the negotiation of the legislative and non-legislative files. Every EU Member State has the obligation to hold the Council Presidency, which changes every six months.
About the CoR
The European Committee of the Regions is the voice of regions and cities in the EU, aiming to reduce the gap between EU institutions’ work and EU citizens. It is composed of more than 350 local and regional elected representatives from across the EU and advises on new laws that have an impact on regions and cities (which is 70% of all EU legislation).
SPONSORS
We are grateful to our sponsors for their generous support of this event.


CONTACT US
Follow this page as well as our Facebook page and Twitter account to see regular updates on this event.
You can get in touch with us at: info@safestroke.eu

Feb 20, 2019
This interview first appeared on European Stroke Association website
 *Professor Anita Arsovska is Head of the Department for Urgent Neurology at the University Clinic of Neurology, University Ss Cyril and Methodius, Skopje, Republic of North Macedonia
*Professor Anita Arsovska is Head of the Department for Urgent Neurology at the University Clinic of Neurology, University Ss Cyril and Methodius, Skopje, Republic of North Macedonia
Professor Arsovska has participated as a subinvestigator in the MARINER and Impact 24B studies. She is an ESO Fellow as well as President of the Macedonian Neurology Society and Board member of Stroke Alliance for Europe (SAFE). She is an active member of the ESO Public Relations and Trials Alliance Committees. Her main interests involve acute stroke management, color duplex sonography and neuroimaging. She is also very active in promoting stroke prevention and raising stroke awareness, organizing many public campaigns and scientific meetings. Prof. Arsovska is involved in the ESO EAST and Angels projects. She also participated in the Action Plan for Stroke in Europe as part of the acute stroke management working group.
What are your main fields of interest in stroke medicine and research?
Many exciting innovations and improvements in the field of acute treatment are taking place, making stroke medicine an energetic discipline. As a Head of the Department for Urgent Neurology, it is my ambition to implement new hyperacute treatments and manage acute stroke patients at the highest level by a multidisciplinary team. I am very honored that I had the opportunity to be a part of the Acute Stroke Management working group in the Stroke Action Plan for Europe 2018-2030 and contribute to fulfillment of the targets for 2030. Beside the acute treatment, I am also interested in stroke prevention and especially in the life after stroke period, a neglected domain in many countries across Europe. Serving as a SAFE (Stroke Alliance for Europe) Board member, gives me an unique opportunity to commit to the needs and rights of stroke survivors and their caregivers and reduce the overall burden of stroke. SAFE, in partnership with ESO has developed the SSOFT – an online learning tool designed to help anyone interested in setting up or developing a Stroke Support Organisation (SSO) in Europe. At the moment, SAFE, in collaboration with ESO is preparing the event ‘Joining forces to prevent and control non-communicable diseases: The role of policy in tackling stroke’, under the patronage of the Romanian Presidency of the Council of the European Union, which will take place on 28 March 2019, in Brussels, at the European Committee of the Regions.
What is the role of ESO in facilitating and promoting the projects you are coordinating or where you are involved?
The European Stroke Organisation (ESO) is a vibrant and dynamic organisation that generously offers many possibilities in networking, education and scientific knowledge. ESO is a true inspiration to its members, providing guidance and sense of belonging to the stroke community. I am truly grateful to currently serve as a member of the PR Committee and Trials Network Committee, and previously in the Membership Committee, thus actively contributing to the mission and vision of ESO. The ESO-EAST initiative is the first comprehensive programme of improving stroke care in Eastern European countries, aiming to harmonize stroke care among all countries in Europe. The Angels Initiative in which I am actively involved is helping us to increase the number of patients in stroke ready hospitals and to optimize the treatment quality for every stroke patient. We have 5 centers registered in the RES-Q registry, an initiative of the ESO EAST Project, a very useful tool for monitoring and evaluation of health care quality, providing insight into specific gaps that need to be improved in our stroke care system.
You can read the full interview here.

Feb 11, 2019
Proios H1, Loutrari A1,4, Tsakpounidou K1, Baskini M1, Uys W2, Van der Merwe J3,
1 Department of Educational and Social Policy, University of Macedonia, Thessaloniki, Greece
2 Lucan Visuals, South Africa
3 Angels Initiative, Boehringer Ingelheim GmbH
4 Aston University, UK
 Growing old comes with wisdom and confidence, but several challenges also come into play. Evidence shows that old age is associated with greater stroke risk (Τeh et al., 2018). But there is always a bright side: old people very often get to enjoy the warm and rejuvenating company of young children. Research shows that during the last decades, the time grandparents spend looking after their grandchildren has substantially increased (Pulgaron et al., 2016). Sharing the process of growing up every step of the way is admirable and heroic. Grandparents are real heroes of the everyday, but even heroes are not invincible. Heroes need their own heroes, so children can become heroes themselves and save the life of their precious grandparents.
Growing old comes with wisdom and confidence, but several challenges also come into play. Evidence shows that old age is associated with greater stroke risk (Τeh et al., 2018). But there is always a bright side: old people very often get to enjoy the warm and rejuvenating company of young children. Research shows that during the last decades, the time grandparents spend looking after their grandchildren has substantially increased (Pulgaron et al., 2016). Sharing the process of growing up every step of the way is admirable and heroic. Grandparents are real heroes of the everyday, but even heroes are not invincible. Heroes need their own heroes, so children can become heroes themselves and save the life of their precious grandparents.
FAST HEROES 112 is an educational program for young children aiming at stroke prevention. Through a five-week pilot stage of the program in Thessaloniki, Greece, children were trained to identify stroke symptoms and seek help by dialing 112. Cartoon heroes representing stroke symptoms and the concept of time were used to familiarize children with the main stroke symptoms and the importance of acting urgently. Preliminary data are encouraging; they show that most children are able to memorize the three main stroke symptoms and appreciate the significance of taking action as fast as possible. FAST HEROES 112 aims to capture the imagination of more children in future interventions and, if need be, turn them into life-saving heroes.
References:
- Pulgaron ER, Marchante AN, Agosto Y, Lebron CN, Delamater AM. Grandparent Involvement and Children’s Health Outcomes: The Current State of the Literature. Fam Syst Health. 2016 September ; 34(3): 260–269. doi:10.1037/fsh0000212.
- Τeh WL, Abdin E, Vaingankar JA, Seow E, Sagayadevan V, Shafie S, Shazana Shahwan S, Zhang Y, Chong SA, Ng LL, Subramaniam M. Prevalence of stroke, risk factors, disability and care needs in older adults in Singapore: results from the WiSE study. MJ Open 2018;8:e020285. doi:10.1136/ bmjopen-2017-020285.

Feb 9, 2019
This article first appeared on ARNI Stroke Charity (UK) website | Author: Tom Balchin
Are you interested in learning about your sleep after stroke?
Researchers at the University of Oxford are currently investigating how sleep is affected by stroke.
Heidi Johansen-Berg is Professor of Cognitive Neuroscience and Director of The Wellcome Centre for Integrative Neuroimaging at the University of Oxford. There, she leads the Plasticity Group whose research focuses on how the brain changes with learning, experience, and damage.
As well as shedding light on how the healthy brain responds to change, The Plasticity Group’s work also has implications for understanding and treating disease. For example, they are currently studying how sleep can affect recovery after stroke.
Would you be interested in learning more about your sleep following stroke?
If so, The Plasticity Group are currently running a study in which you might be interested in participating – or you may know someone who is.
The aim for this study is to investigate how sleep is affected by stroke which could help to develop better sleep improvement programmes specifically for individuals after stroke.
We know that sleep plays an important role in learning. Studies have shown that if you take two groups of people and teach them the same skill, such as juggling, then allow one group to sleep for a few hours and keep the other group awake, the sleep group will perform significantly better when retested as they have been able to consolidate the memories of learning the skill through sleep.
Learning, or re-learning, of motor skills is a key component of motor rehabilitation after stroke. If sleep is impaired following stroke then consolidation of motor skills gained through physical rehabilitation may be diminished. Therefore, finding out about how sleep is affected by stroke could help us to develop better rehab outcomes following stroke.
The current study involves coming to a research centre in Oxford for one session to complete a couple of motor assessments with the upper limbs and to answer a couple of questionnaires about your sleep and mood. Then researchers will set you up with a pair of sleep monitoring wrist watches for you to wear for a week with a simple sleep diary asking what times you go to bed and get up each day.
Read the full article here.

Feb 7, 2019
The Angels Initiative is a unique healthcare initiative launched by Boehringer Ingelheim in partnership with the European Stroke Organisation (ESO), the World Stroke Organisation (WSO) and the Stroke Alliance for Europe (SAFE).
SAFE’s members proudly contributed to the Angles Initiative by providing critical information to stroke patients and their families as early as in stroke units. In addition to containing useful and evidence-based information, these brochures help improve patient – doctor communication as well.
The SAFE Angels project was realised in the first half of 2018. It involved translation to 13 European languages, design, printing and distribution of five different brochures for stroke patients and their carers. The core texts were kindly provided by Stroke Association UK.
13 organisations from the following countries took part in this project and made sure these brochures were made available in the stroke units: Spain, Serbia, Poland, Czech Republic, Latvia, Croatia, Macedonia, Greece, Ukraine, Georgia, Hungary and Turkey.
Patient information brochures are available only in a selected number of hospitals in the project countries, but can also be downloaded from SAFE website.
“We consider this as a pilot project, because we already distributed the whole quantity of the patient information brochures and now both patients and medical staff are asking when we will have it again. For now, we are signposting people to visit SAFE’s website and download the PDF versions.”
Ivan Milojevic, Serbian stroke support organisation Mozdani udar
In 2018, the Angels Initiative won the prestigious 2018 EFPIA Health Collaboration Award for Improving Stroke Care.
Deciding among 80 other applications, the European Federation of Pharmaceutical Industries and Associations (EFPIA) decided to honor the Angels Initiative with a “Health Collaboration” award in the category Service Delivery.
SAFE members proudly reported about this event, reminding their audiences once again of when these brochures can still be found in 12 European countries. For more detailed information, please see our Facebook page or look up for a specific stroke support organisation’s Facebook profile.





 “I set a sign.”
“I set a sign.” The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters.
The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters. The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke.
The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke. The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning:
The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning:








 *Professor Anita Arsovska is Head of the Department for Urgent Neurology at the University Clinic of Neurology, University Ss Cyril and Methodius, Skopje, Republic of North Macedonia
*Professor Anita Arsovska is Head of the Department for Urgent Neurology at the University Clinic of Neurology, University Ss Cyril and Methodius, Skopje, Republic of North Macedonia
 Growing old comes with wisdom and confidence, but several challenges also come into play. Evidence shows that old age is associated with greater stroke risk (Τeh et al., 2018). But there is always a bright side: old people very often get to enjoy the warm and rejuvenating company of young children. Research shows that during the last decades, the time grandparents spend looking after their grandchildren has substantially increased (Pulgaron et al., 2016). Sharing the process of growing up every step of the way is admirable and heroic. Grandparents are real heroes of the everyday, but even heroes are not invincible. Heroes need their own heroes, so children can become heroes themselves and save the life of their precious grandparents.
Growing old comes with wisdom and confidence, but several challenges also come into play. Evidence shows that old age is associated with greater stroke risk (Τeh et al., 2018). But there is always a bright side: old people very often get to enjoy the warm and rejuvenating company of young children. Research shows that during the last decades, the time grandparents spend looking after their grandchildren has substantially increased (Pulgaron et al., 2016). Sharing the process of growing up every step of the way is admirable and heroic. Grandparents are real heroes of the everyday, but even heroes are not invincible. Heroes need their own heroes, so children can become heroes themselves and save the life of their precious grandparents.