Dec 21, 2018
Oruen – The CNS Journal has now been published online. In this issue you can find the SAFE special report on stroke prevention project and Stroke Action Plan for Europe advert. SAFE is also mentioned in the two ANGELS articles.
The current issue also brings you the following reviewed articles:
Clinical Outcomes and Work Flow Optimisation with Pipeline System and Shield Technology (Istvan Szikora, Saleh Lamin, Mohamed Aggour)
Innovations in Endovascular Treatment of Acute Ischemic Stroke and Cerebral Aneurysms (Hannes A. Deutschmann, Marc Ribo, Mathieu Sanchez)
The ANGELS Initiative: More and better Stroke-ready Hospitals across the globe (Rob Goodwin)
Improving stroke care across the world: The Angels Initiative (Valeria Caso, Magd Fouad Zakaria, Ales Tomek, Robert Mikulik, Sheila Cristina Ouriques Martins, Thang Huy Nguyen, Anastasia Rossouw)
Stroke Prevention in atrial Fibrillation: update with NOAC Treatment and the impact of Reversal (Dr. Allison Kirsop)
Transition of ADHD Patients from Childhood into Adulthood (Dr Allison Kirsop)
An Introduction to the Internal Capsule in Schizophrenia (Dr. Matthew Williams)
About Oruen – The CNS Journal
The journal is owned and published bi-annually by Oruen Limited; it is a peer-reviewed, open access publication, and has received CME accreditation from the European Accreditation Committee in CNS (EACIC) with a 100% focus on original CNS research topics, and the latest advances, diagnoses, and treatment of CNS disorders. Oruen – The CNS Journal is distributed in print and electronically to thousands of physicians, researchers, academics, nurses, and related healthcare professionals with an interest in CNS disorders. Both subscription and access are free and there are no contributory author fees for publication. Papers submitted for publication are accepted based on their originality, likely impact on and relevance to clinical practice, data quality, and overall potential interest to the journal’s readership.

Dec 20, 2018

Dec 14, 2018
First published on ScienceDaily.com
Aggressive treatment of hypertension in stroke patients could do more harm than good in the long term, according to a new study from researchers at the University of Georgia.
Sixty percent of stroke patients admitted to U.S. emergency rooms have elevated blood pressure, and many studies say that having high blood pressure at the time of stroke can lead to higher rates of death and major disability.
But lowering blood pressure too much with medications may actually be working against the body’s protective response to maintain blood flow into the affected brain tissues.
“This presents a clinical dilemma,” said study author Changwei Li, an assistant professor of epidemiology and biostatistics at UGA’s College of Public Health.
It may be better to keep blood pressure a little higher than normal, closer to 140/90 mmHg rather than a “good” blood pressure of 120/80 mmHg, but that leaves the question of best practices a little open-ended.
“Currently, hypertension treatment for acute stroke patients is based on physicians’ clinical experience and judgement,” said Li. “There is no guideline on how low the blood pressure should be maintained.”
The key is to find the right balance between maintaining blood flow to the brain and reducing negative short- and long-term effects.
To help identify this optimal blood pressure, Li and his co-authors looked at the relationship between blood pressure during stroke and both short- and long-term health outcomes for over 4,000 Chinese stroke patients participating in the China Antihypertensive Trial in Acute Ischemic Stroke study. One group of stroke patients received extensive treatment for high blood pressure while a control group received no treatment at the time of their stroke.
Li and his collaborators tracked blood pressure changes over time in both the treatment and control groups during the first week of hospital admission and compared patient health at one week, three months, one year and two years following the stroke across patients of different blood pressure trajectories.
To access the full article, please click here.
Story Source:University of Georgia. “Optimal blood pressure treatment for stroke patients.” ScienceDaily. ScienceDaily, 10 December 2018. <www.sciencedaily.com/releases/2018/12/181210142059.htm>.

Dec 8, 2018
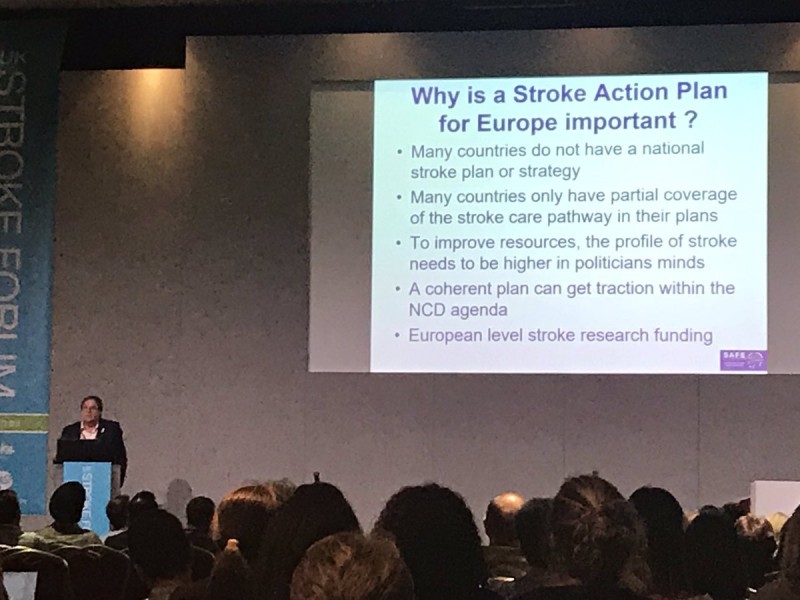
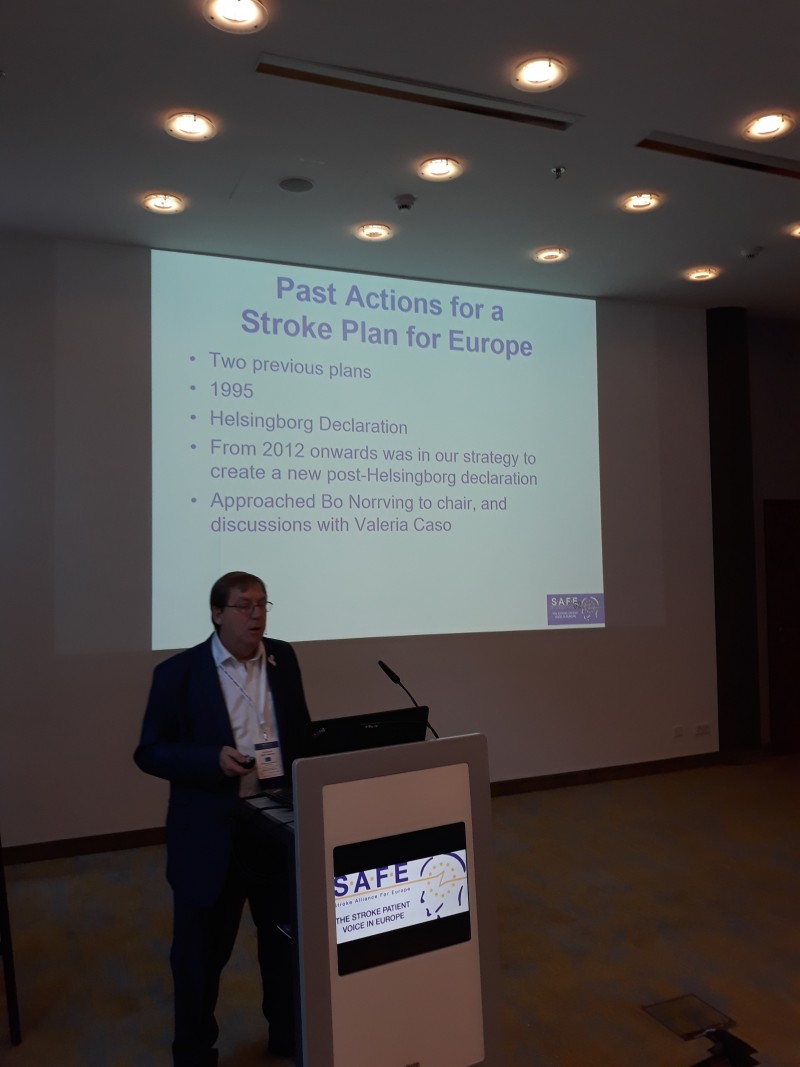
Jon Barrick, SAFE President, presented Stroke ACtion Plan for Europe 2018-2030 at the 13th UK Stroke Forum Conference (#UKSF18). The #UKSF18 took place at The International Centre, Telford,UK, from 4 – 6 December 2018.
“There was a great need for a document such as the Stroke Action Plan for Europe. Many European countries do not have a national stroke plan or strategy and many of them only have partial coverage of the stroke care pathway in their plans” said Barrick.
This 3 day multidisciplinary conference brought together over 110 expert speakers and researchers, all committed to improving stroke care.
About UK Stroke Forum
The UK Stroke Forum is a coalition of over 30 organisations all committed to improving stroke care in the UK. The coalition is underwritten by the Stroke Association UK.
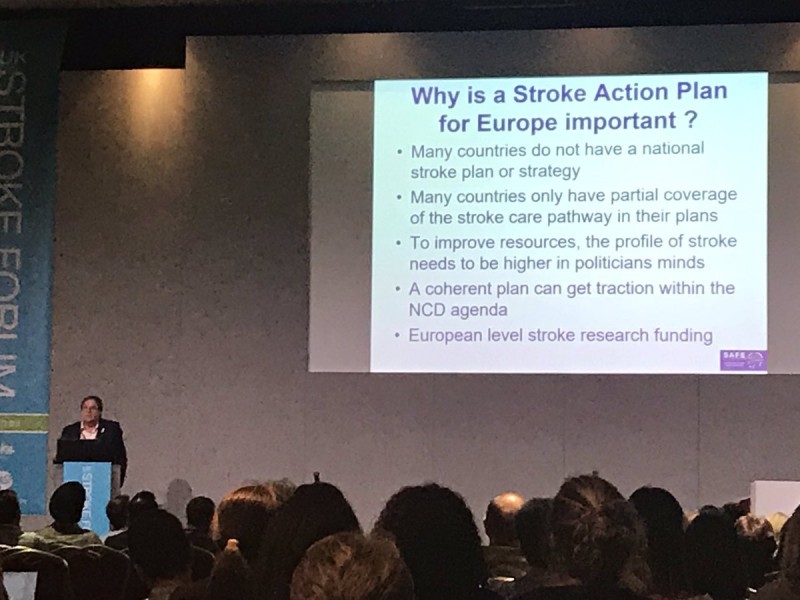
Photo by Sarah Belson

Dec 4, 2018
Roman Shwed from Ukraine is a stroke survivor and a first-time attendee at SAFE Working Conference in Berlin. He shared with us his unique view of this event, kindly agreeing that we share it further with the world. We at SAFE believe you will enjoy it… (In the photo above, Roman Shwed is the first person on the left).
A “TOUNGUE IN CHEEK”, SHORT REPORT ‘SO TO SPEAK’, OF MY WONDERFUL EXPERIENCES IN THE CITY OF BERLIN, GERMANY, NOT TO BE CONFUSED WITH BERLIN, NEW JERSEY, OR ANY OTHER BERLIN ON THE PLANET…
…anyway,
I’m talking about our “SAFE 2018 WORKING CONFERENCE”, which was masterfully dreamed up, programmed, and prepared, by Jon Barrick, the Prez., his VP Markus Wagner, plus Secretary Monique Lindhout, Treasurer Grethe Lunde, Board Members Ivan Milojevic’, Anita Arsovska, Pnina Rosensweig, Kolbrun Stefansdottir, and on the 27th through 30th November, professionally executed by the staff which included Sandra Jackson, Lucinda Shaw, Gary Randall, Jelena Misita, and Victoria Brewer. If I missed anyone, or misspelled a name, kindly forgive my mistakes…this was the very first, never ever before attended, SAFE Working Conference in my whole life, and I meticulously copied all that info from the SAFE Annual Report…so there !
…but I digress,
If anyone has any doubts about my feelings about this conference, let me tell you, I was duly impressed, wow-ed, amazed, and, …in a word, the conference “knocked my socks off” ! I learned a bunch of new stuff about “Life after Stroke”, and reflected on my own situation. What kind of Stroke did I experience ? After seeing all the Delegates, especially other Stroke survivors, and remembering what the 3 types of Stroke are, namely: Ischemic, Hemorrhagic, and TIA, my opinion about my Stroke changed dramatically.
Now when friends on the street will ask me, “Roman, why do you walk so funny ?”, I’d explain that “Moi had a Stroke”…then they usually asked me, politely, “oh?… what kind of Stroke was it ?”, showing off their assumed Stroke knowledge. I used to be very exact in my replies, telling them that it was an Ischemic Stroke, and then, the questioner would, invariably, nod his or her head, sympathetically. Well, this routine is changing, and from now, when asked, I will tell them, “I had STROKE LIGHT ”, for which they’ll have no smarty pants reply, and also this will, hopefully, generate no additional questions. I did, for a while, consider calling mine the Diet Coke way, like “DIET STROKE”, but it just wasn’t sexy enough.
…but, again, I digress,
My friend Dr.Dmytro Gulyayev, (my Ukrainian co-conspirator), who took care of my Stroke recovering body, introduced me to Sandra, and we immediately became friends, but then small wonder, everyone else who was there accepted me and my ‘Drunken Sailor’ walk without question. It’s really comforting to be among people that understand what you went through, and are still, like you, overcoming this health burp in their life. The Conference was peopled by Delegates from “almost” all European Countries, but everyone spoke English…well, let me clarify. There is the Queen’s English, as spoken by Jon, Sandra, and a few others, then there was some Brogue English, as spoken by my Irish & Northern Irish friends, a little North American English, like mine, and the rest spoke European, or as I fondly refer to, YODA English. Yoda would be very proud of us all, because every single Delegate is battling the DARK STROKE Force like a true Jedi Knight !
…but I can’t help myself…I still digress,
As the second day came into play, Integrated Care in Germany was presented by Markus Wagner, our V.P., and then Michael Brinkmieir, the Chairman of the German Stroke Foundation, had a very good presentation of Case & Care Management in East Westphalia. Our table started to speculate…”if there is a Westphalia, there must be an Eastphalia, and therefore – a West Eastphalia”…but we never reached a final agreement, so if you have any doubts, just GOOGLE it. Anyway, the Workshops were great, and very useful, especially to a “nebish” like me. Dmytro and I were there to Listen & Learn, and our East Cluster Workshop, which was in Hamburg…the Room, not the Burg, explained our moderator, and allayed our fears of having to travel to another City.
If I have any complaints, it’s about the food. The meals were great, tasty, and I think that I must have gained a kilo or two. It just isn’t fair to guy’s like me, when you place such tasty temptations before us. The Wednesday Night Feast at Maximillian’s was superb, and I’m sure that our ladies enjoyed the waiters in “Lederhosen”. I believe that everyone, Staff and Jedi Knight, had 2 pretzels each, but who cares as long as no one broke into song or yodelling.
ALL THAT’S LEFT TO SAY IS A GREAT BIG THANK YOU TO THE LEADERSHIP & STAFF OF SAFE, AND OUR WONDERFUL SPONSORS … “THANK YOU” IS CERTAINLY AN UNDERSTATEMENT…BECAUSE MY VOCABULARY IS TOO LIMITED TO DO JUSTICE TO THE BERLIN CONFERENCE,
AND I MUST ADD A HEARTFELT – “YO, AND A FIST BUMP”, THANK YOU DELEGATES – JEDI KNIGHTS ALL … MAY THE “SAFE” FORCE BE WITH YOU !
I DID MEET SOME OF YOU PERSONALLY, AND LOOK FORWARD TO MEETING THE REST OF YOU REAL SOON !
SMILINGLY YOURS,
Roman “Toungue in Cheek” Shwed,
UKRAINE

Dec 2, 2018
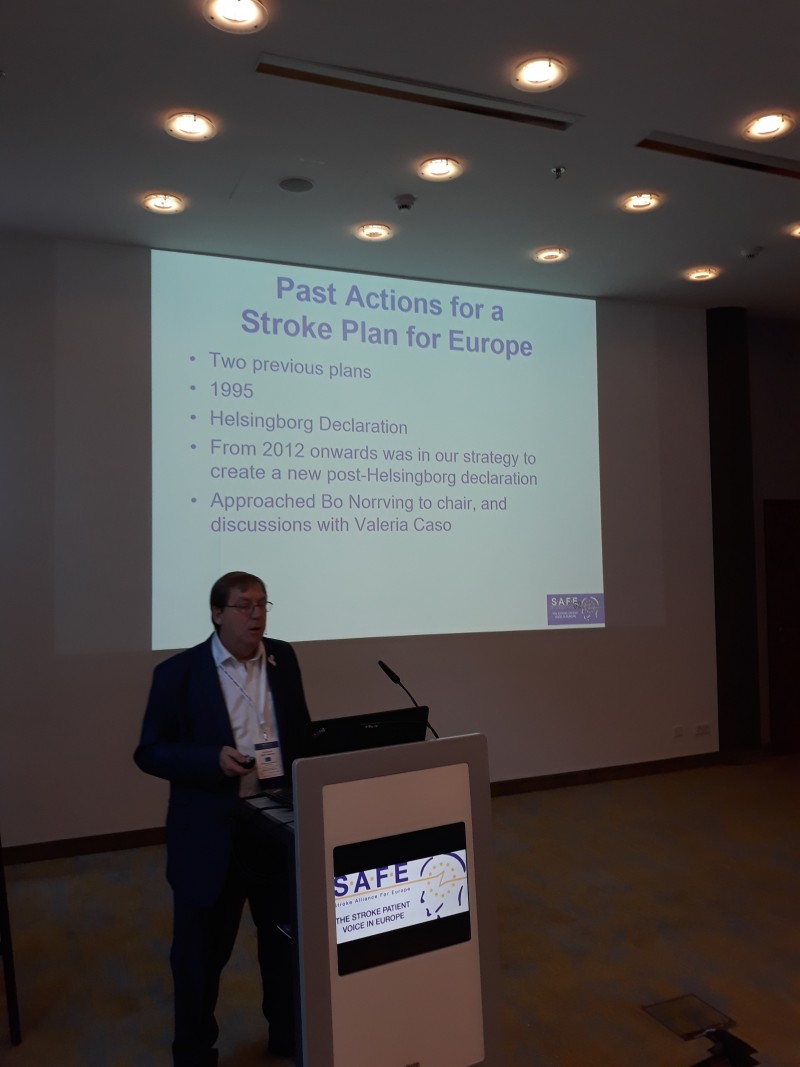
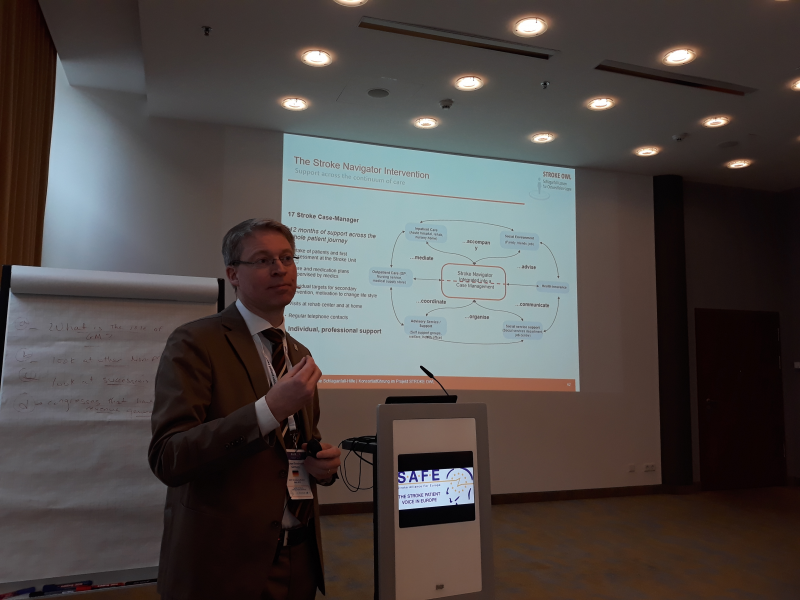
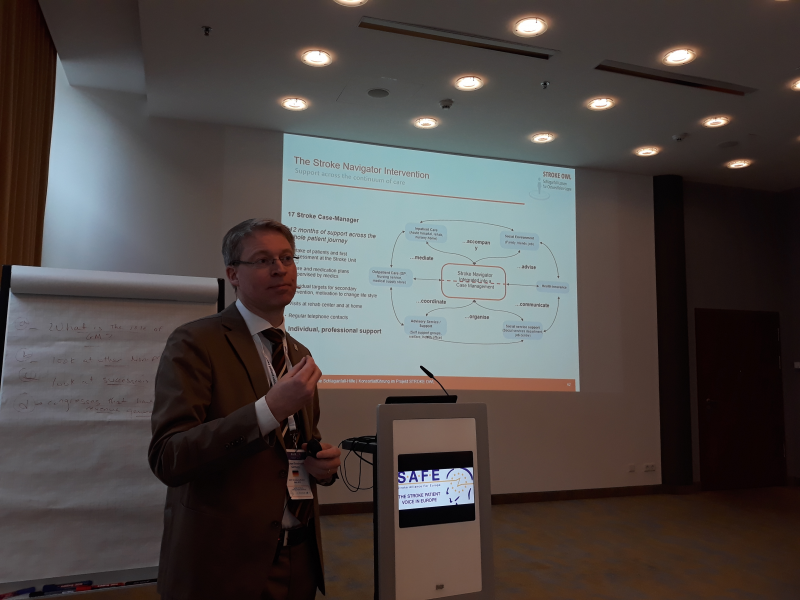
SAFE held this year’s Working Conference and the General Assembly in Berlin, Germany. The event was very well attended, with over 100 delegates and representatives of SAFE’s industry partners.
The hosting organisation was the Stiftung Deutsche Schlaganfall Hilfe, SAFE’s member organisation from Germany, whose President, Michael Brinkmeier presented their latest projects to the auditorium. SAFE President Jon Barrick and ESO Board member Heinrich Audebert gave presentations on how the Stroke Action Plan for Europe 2018-2030 was created, including the overarching recommendations on the seven domains, from Primary Prevention to Life After Stroke.
The working conference was dedicated to updating our members on the current projects and presenting plans for the next period, until 2020 and beyond.
Stroke Support Organisation Faculty Tool was completed just before the SAFE’s annual gathering and SSOFT Project Director, Victoria Brewer gave a wrap up, summarizing the achievements and giving recommendations for future use and increased engagement.
You can access the complete Working Conference Agenda here.
On Friday, 30th November, SAFE had a General Assembly. Three new Board members were elected: Grethe Lunde from Norway (Norsk forening for slagrammede (NFS)) as a North Cluster Representative, Chris Macey from Ireland (Irish Heart Foundation) as Treasurer and Marina Charalambous from Cyprus (Cyprus Stroke Organisation) as Board Member at Large.

Two new organisations were ratified and became full SAFE members: Porážka.sk from Slovakia and CEREBRUM from Czech Republic.
SAFE awarded stroke support organisations from the following countries: Turkey, Spain, Serbia,Croatia, Portugal, Iceland and Cyprus for their work in fighting stroke, supporting survivors and their families and building the patient voice during 2018.

In addition, SAFE Annual Report and Strategy were discussed, as well as the upcoming SAFE political activities at EU level.





Nov 30, 2018
Stroke can happen to anyone, anytime. We spoke with Hrvoje Jurlina, MD, who has a unique perspective on stroke, being a medical professional, a young stroke survivor and a caregiver who recently lost his father to stroke. Hrvoje Jurlina is the Second Vice-President of Croatian Stroke Society, which is a SAFE member.
Please click on the picture below to access the audio file.


Nov 26, 2018
First published on ScienceDaily.com
Some patients with coronary artery disease have inadequate blood flow to the heart muscle during periods of mental/emotional stress. This condition — called “mental stress-induced myocardial ischemia” (MSIMI) — is related to the severity of plaque buildup in the coronary arteries in men but not women, reports a study in Psychosomatic Medicine: Journal of Biobehavioral Medicine, the official journal of the American Psychosomatic Society. The journal is published in the Lippincott Portfolio by Wolters Kluwer.
Mental stress-induced myocardial ischemia occurs in both men and women, although younger women tend to have more of this phenomenon. While MSIMI is linked to worse cardiovascular outcomes in both sexes, there may be sex differences in the mechanism through which stress can trigger MSIMI, according to new research by Viola Vaccarino, Md, PhD, and colleagues, of Emory University School of Public Health and School of Medicine, Atlanta.
Heart Response to Stress Linked to Coronary Plaque Severity in Men, but Not Women
The researchers examined the sex-specific association between coronary plaque buildup (obstructive coronary disease) assessed from angiograms and MSIMI in 276 participants — 141 men and 135 women — with recent myocardial infarction (heart attack). The study targeted young and middle-aged adults (under age 61). All participants underwent conventional stress testing to evaluate myocardial blood flow in response to a physical or pharmacological challenge (either an exercise stress test or a pharmacological stress test) .
The patients also underwent a mental stress test, which evaluated myocardial blood flow in response to a stressful situation (a public speaking task). Based on a reduction in myocardial blood flow during this stressful challenge, 17 percent of patients were classified as having MSIMI.
Women had a higher rate of MSIMI (20 percent) than men (15 percent). Twenty-seven percent of patients had conventional stress-induced myocardial ischemia (CSIMI). Only 10 percent of patients had both MSIMI and CSIMI.
In both men and women, the presence of CSIMI was associated with greater obstructive coronary disease severity. For each one-unit increase in severity score, the likelihood of CSIMI increased by about 50 percent, after adjustment for other factors.
In contrast, the presence of MSIMI was associated with more severe plaque buildup only in men: for each one-unit increase in severity score, the likelihood of MSIMI nearly doubled. For women, MSIMI was unrelated to obstructive coronary disease severity.
“There is growing evidence that psychosocial stressors may promote the development and progression of cardiovascular disease in susceptible individuals,” according to the authors. However, the relationship between MSIMI and obstructive coronary disease, which means blockages in the major coronary arteries supplying blood to the heart muscle, has been unclear. Women are more likely than men to develop myocardial ischemia without coronary obstruction.
The results support the hypothesis that MSIMI may develop via different mechanisms in women versus men. Consistent with previous findings on sex differences in heart disease, it may be that MSIMI in women mainly reflect abnormalities other than blockage of the coronary arteries, such as malfunction of the smaller coronary blood vessels (microcirculatory dysfunction).
The sex differences may have important implications for understanding sex-specific vascular effects of psychological stress in general and the mechanisms of MSIMI in particular, since most previous studies of this issue have focused on men. Dr. Vaccarino and colleagues conclude, “These results suggest that MSIMI must be driven by alternative mechanisms especially among women, and provide motivation for further research to understand sex-specific mechanisms for the effects of mental stress on myocardial ischemia and long-term outcomes.”
Story Source:Wolters Kluwer Health. “Stress-induced effects on heart blood flow differ for men versus women.” ScienceDaily. ScienceDaily, 26 November 2018. <www.sciencedaily.com/releases/2018/11/181126154101.htm>.

Nov 24, 2018
On November 22nd, 2018 EFPIA (The European Federation of Pharmaceutical Industries and Associations) announced winners of this year’s Health Collaboration Award. The overall winner is the Angels Initiative project.
With over 80 entries received from across Europe, The Health Collaboration Awards gives an opportunity to showcase collaborative projects that have benefitted the lives of patients across Europe. Giving her reaction, EFPIA Director General, Nathalie Moll said “As we seek to address the challenges faced by patients and our healthcare systems, partnership and collaboration will be key. No one sector has all the answers and by putting patients at the heart of projects, pooling our resources and expertise and finding new, innovative ways of addressing health needs it is amazing what we can achieve. The entries and winners of this year’s Health Collaboration Awards are fantastic examples of that approach and I hope will provide food for thought and inspiration to us all.”
SAFE is proud to be part of the Angels Initiative project, providing critical information to stroke patients when they most need it, already in the stroke unit. SAFE’s contribution to this amazing project started in May this year simultaneously in 12 European countries: Spain, Serbia, Poland, Czech Republic, Latvia, Croatia, Macedonia, Greece, Ukraine, Georgia, Hungary and Turkey.
In selected hospitals in these countries, stroke patients and their carers will be provided with information on stroke and important next steps on their path to recovery. The patient-focused materials are made of five brochures, including a list of national, regional and local stroke support organisations, with their contact details, in order that patients and carers can access further support in the months and years following their stroke. The information provided in the brochures are kindly provided by the Stroke Association UK and then translated to all project languages, applying the information standard procedure for the translation.

About EFPIA
The European Federation of Pharmaceutical Industries and Associations (EFPIA) represents the pharmaceutical industry operating in Europe. Through its direct membership of 36 national associations and 40 leading pharmaceutical companies, EFPIA’s mission is to create a collaborative environment that enables our members to innovate, discover, develop and deliver new therapies and vaccines for people across Europe, as well as contribute to the European economy. Our vision is for a healthier future for Europe. A future based on prevention, innovation, access to new treatments and better outcomes for patients.
About Angels Initiative
Every 30 minutes a stroke patient who could have been saved, dies or is permanently disabled, because they were treated in the wrong hospital.
Angels Initiative is building a global community of stroke centres and stroke-ready hospitals, working every day to improve the quality of treatment for every stroke patient.
The goal is to get 1500 stroke-ready hospitals around the world by May 2019.
For more information about Angels Initiative, please visit www.angels-initiative.com

Nov 21, 2018
Brussels, 21st November 2018 – As the second biggest killer in the world, the response to Stroke needs an army of advocates to ensure the message that it is preventable, treatable and beatable is implemented. SSOFT is an excellent tool to educate people on the principles of stroke advocacy. It will strengthen their ability to advocate for better stroke prevention, treatment and after care. This module is vital as a contribution to effective public campaigning. We believe that SSOFT will provide inspiration for future stroke advocates to make a real-life change, says Jon Barrick, SAFE President.
The sixth and final eLearning module of the Stroke Support Organisation Faculty Tool (SSOFT) is published today at the following address www.ssoft.info, thus marking the completion of this innovative eLearning tool on stroke support organisation and the principles of stroke advocacy.
The SSOFT’s sixth module focuses on the skills and principles around developing effective public advocacy campaigns.
SSOFT’s development and execution was successfully led by Victoria Brewer, SAFE Project Director, who stressed from the beginning of the project that the members of the SAFE had to be central to the whole process. SAFE members have been actively involved in the development of the content by either testing the modules, providing cases studies or sharing their experience in interviews. These examples have brought much of the content to life by providing real world cases studies of how the knowledge contained in the modules can be applied.
“The opinion of the people who test the program [has been] important. Therefore, SSOFT is exactly what should be: a tool ‘for our members by our members’.” Nenad Nikolić Moždani Udar, the Serbian Stroke Association
The release of the final module marks a significant stage in SSOFT’s development with this stage of development being completed. SAFE is currently exploring future expansion options for SSOFT
“I hope that the tool will never be truly “finished” but remain a live environment that always adapts to the latest developments and experiences.” André de Rosa Spierings, National Board member of Hersenletsel, Netherlands.
About SSOFT’s 6th module
SSOFT’s sixth module focuses on the skills and principles around developing effective public advocacy campaigns. The module is broken down in to five bitesize sections, which cover:
6.1 Public advocacy – focuses on the role of public engagement in advocacy & how to dispel stroke myths to drive change.
6.2 Stroke Community & Mass Campaigning – covers how to build a stroke community & campaign to a large audience
6.3 Publicity – demonstrates how to manage publicity by engaging with print & broadcast media
6.4 Traditional Media – helps learners to understand the role of traditional media &and learn how to work with journalists & editors
6.5 Social Media – examine the role of social media in bringing momentum for change.
About SSOFT
SSOFT is an innovative online eLearning advocacy tool being developed by Stroke Alliance for Europe (SAFE), in partnership with the European Stroke Organisation (ESO).
“I think this is just the beginning; …. I envisage this resource as further strengthening the European stroke patient network and in time the global stroke patient network.” @BelsonSarah
This online learning platform provides knowledge and training on how the creation of effective advocacy activities and campaigns to deliver positive change at a local and national level on stroke prevention, treatment and care. The eLearning platform includes six modules that provide information on:
Module 1: Stroke Support Organisations (SSOs)
Module 2: Making Change Happen
Module 3: Use of Evidence
Module 4: Role of Patient Voice
Module 5: Health & Care System Advocacy
Module 6: Public Advocacy
The modules and learning environment are accessible via the SSOFT website through a simple registration process. Visitors to the website can also learn more about SSOFT, SAFE and ESO, find their nearest SAFE Stroke Support Organisation (SSO) as well as hear from SAFE members about their experiences.
For more information, please send an email ssoft@safestroke.eu or visit www.ssoft.info
Acknowledgments
SAFE would like to take this opportunity to thank and acknowledge the contributions made by those who have helped in the development of SSOFT and module 6.
Stroke Alliance for Europe Board, who have been involved at every stage of development of this module.
The Peer Reviewers for module 6:
- Stiftung Deutsche Schlaganfall-Hilfe (Dr Markus Wagner)
- World Stroke Organization (Anita Wiseman)
- Irish Heart Foundation (Chris Macey)
- Different Strokes Charity (Austin Willets)
- Hellenic Alliance/Action for Stroke Support Organization (Dr Hariklia Proios)
- Macedonian Stroke Association (Dr Anita Arsovska)
Our members who have shared their experiences and knowledge in the video interviews used within the module:
- Adam Siger – Fundacja Udaru Mózgu, Poland
- Anita Arsovska – Macedonian Stroke Association
- Chris Macey – The Irish Heart Foundation, R.Ireland
- Hrvoje Jurlina – HDPMU Croatian Stroke Society, Croatia
- Francesca Romana Pezzella – ALICe, Italy
- Jon Barrick – Stroke Alliance for Europe (SAFE)
- Mara Cochetti – ALICe, Italy
- Nenad Nikolić – Moždani Udar, Serbia
- Pnina Rosenzweig – Neeman Association for Stroke Survivors, Israel
Our member and partner organisations who have collaborated in the development of the module content:
- World Stroke Organization
- European Stroke Organisation
- Stroke Association UK
And all those who participated in the User Acceptance Testing of module 6.
We would also like to thank the project sponsor Bayer Healthcare who have supported this project through an education grant.
About SAFE
The Stroke Alliance for Europe (SAFE) a non-profit-making organisation formed in 2004. It is the voice of stroke patients in Europe, representing a range of patient groups from 30 European countries.
SAFE’s goal is to decrease the number of strokes in Europe by advocating for better prevention, access to adequate treatment, post-stroke care and rehabilitation.