Aug 31, 2018
Death and illness caused by noncommunicable diseases bring suffering and heartache to millions of people worldwide every year – those who live with the diseases, as well as their families and friends. 70% of all deaths worldwide result from NCDs.
In light of the upcoming Week For Action on NCDs Activities & Comms within the ‘Enough.’ campaign, we used an opportunity to talk with Jelka Jansa, from the Stroke Support Organisation Slovenia. Jelka recently participated in a NCD Alliance workshop in Geneva and being an occupational therapist who works in an acute neurological hospital, she is very familiar with patient support organisations both locally and internationally, especially in the field of stroke.
What is ‘Week For Action on NCDs’ and when is it happening?
It takes place on the 3-9th September. As part of the Enough campaign, the NCD Alliance is encouraging the NCD community all over the world to observe a Global Week of Action on NCDs from the 3rd to 9th of September 2018 in the lead up to the UN HLM on NCDs which will take place later that month on the 27th September. The Global Week for Action on NCDs will catalyse activity among people who are engaged in the NCD movement everywhere, to initiate a transition from commitment to action on NCDs and we encourage you to get involved individually or through your country NCD alliances, in a way that works for you in your context, based on available resources, capacities and priorities.
This will be a global opportunity to talk to each other, to leaders, to media, to crowds, to the world about what works well and what needs to change to ensure a transition from commitment to tangible actions that not only yield reportable improvements in NCD targets and outcomes, but result in the improvement of health and lives of all people in all places.
The opportunities are endless. Possible activities include organising a meeting, street action, picnic, fun run, dance party, art competition or social media support. The week is your chance to do something achievable, appropriate, relevant and impactful where you live, but linked to a global movement. Saying ENOUGH is also a nice way of participating.
Objectives:
-
Show solidarity and a strong united civil society movement to address NCDs globally
-
Draw attention to the UN HLM on NCDs
-
Mobilise around the ENOUGH campaign and emphasise that we all say ENOUGH. Our HEALTH, is our RIGHT, and we need action NOW.
The Global Week for Action will be led by NCD Alliance, with collaborative support of the WHO Civil Society Working Group on NCDs, partners, members, supporters and wider NCD civil society network.
The Guide for Planning your Week for Action on NCDs, Activities and Comms is available for free at this link. It includes useful tips and checklists to help in your planning over the coming three weeks. To complement the guide, you can also find a suite of editable graphics for social media (with English and Spanish versions) to help to promote the Global Week for Action on NCDs and support your activities here.
WHAT HAVE YOU HAD ENOUGH OF?
Share your views and make your own pledge to help stop preventable death and suffering ahead of the 2018 UN HLM on NCDs.
TELL THE WORLD

Aug 31, 2018
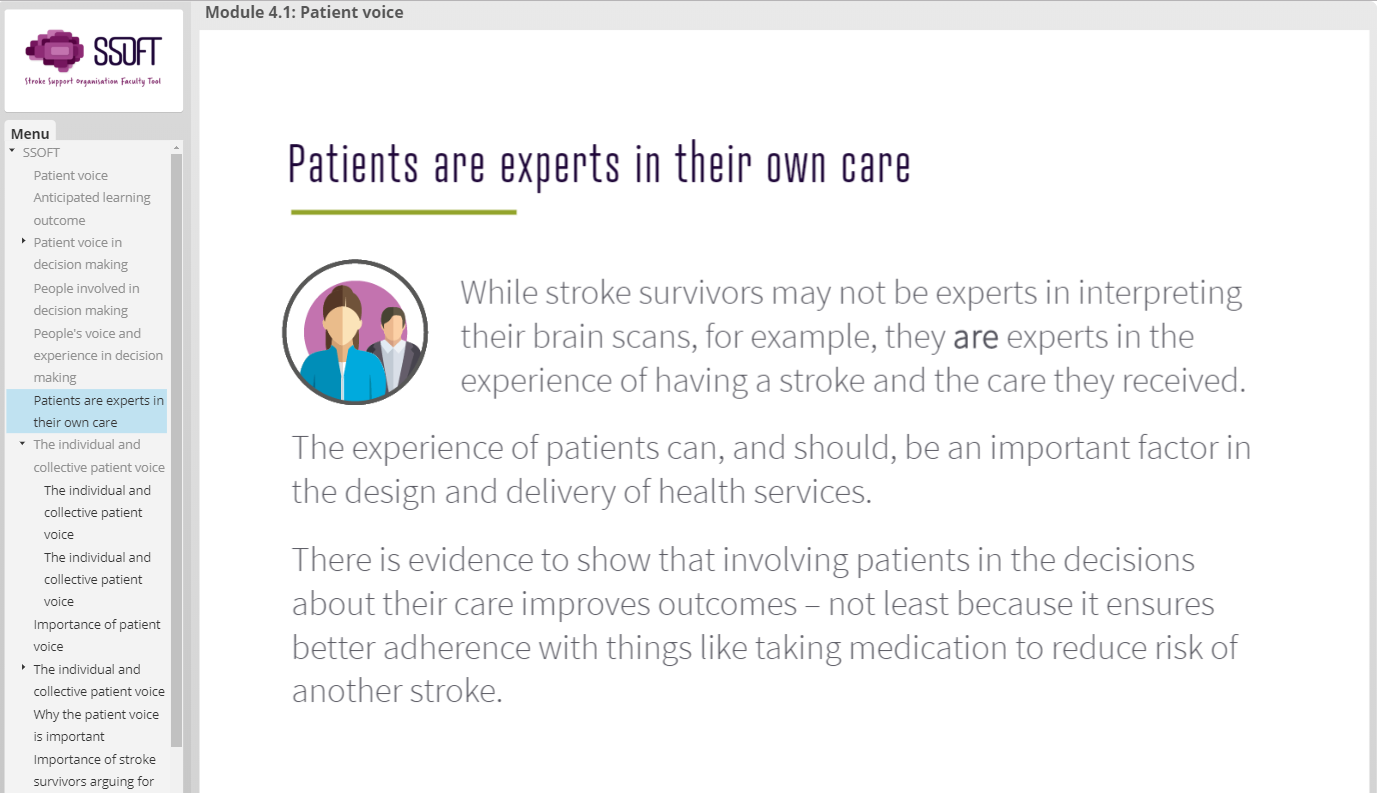
Brussels, 31st August 2018 – The eLearning Module 4 of the Stroke Support Organisation Faculty Tool (SSOFT) is published today at the following address www.ssoft.info.
In Module 4, using a combination of theory and practice, SSOFT demonstrates the impact of the individual and collective patient voice. Learners will develop an understanding for the role of the stroke patient and survivor in research and development of stroke guidelines; and how to argue for patient involvement and rights in the context of regulatory, ethical and advisory processes.
SSOFT’s fourth module focuses on what rights patients have and how the voice of the stroke survivor and their families can be used ethically to support SSOs causes and campaign.
The module is broken down in to five bite-size sections, which covers:
4.1 – Patient voice
4.2 – Patient voice in research
4.3 – Patient voice in guideline development
4.4 – Institutional processes impacting on the patient voice
4.5 – Patient’s rights
Stroke Support Organisations have been at the heart of this tool. For newer or smaller organisations, the information in the tool will provide knowledge that will help them build their capacities and grow. Larger organisations will be enabled to support their communities and other stroke professionals across Europe and add more voices to their movement/arguments for change.
This tool is also for anyone who is interested in knowing more about what an SSO is, how to start and develop one and how to make it sustainable.
For those interested in using this innovative eLearning platform we would encourage them to visit the SSOFT website www.ssoft.info
This online learning platform provides knowledge and training on how the creation of effective advocacy activities and campaigns to deliver positive change at a local and national level on stroke prevention, treatment and care. The eLearning platform will include six modules that provide information on:
About SSOFT
SSOFT is an innovative online eLearning advocacy tool being developed by Stroke Alliance for Europe (SAFE), in partnership with the European Stroke Organisation (ESO).
Module 1: Stroke Support Organisations (SSOs)
Module 2: Making Change Happen
Module 3: Use of Evidence
Module 4: Role of Patient Voice
Module 5: Health System Advocacy
Module 6: Public Advocacy
The modules and learning environment is accessible via the SSOFT website through a simple registration process. Visitors to the website can also learn more about SSOFT, SAFE and ESO, find their nearest SAFE Stroke Support Organisation (SSO) as well as hear from SAFE members about their experiences.
For more information, please send an email ssoft@safestroke.eu or visit www.ssoft.info
Acknowledgments
SAFE would like to take this opportunity to thank and acknowledge the contributions made by those who have helped in the development of SSOFT and Module 4.
Stroke Alliance for Europe Board, who have been involved at every stage of development of this module.
The Peer Reviewers for module 4:
• Stiftung Deutsche Schlaganfall-Hilfe (Dr Markus Wagner)
• Hellenic Alliance/Action for Stroke Support Organization (Dr Hariklia Proios)
• Macedonian Stroke Association (Dr Anita Arsovska & Dr Maja Bozinovska Smiceska)
• Norsk forening for slagrammede (Ms Grethe Lunde)
• Thessaloniki and Wiesbaden NRZ, Rehabilitation Center Germany (Dr Dimitris Artemis)
• Aristotle University, Greece (Dr Katerina Nicolaidis)
• Anagenissis Rehabilitation Center, Greece (Ms Eugenia Stamatiou)
Our members who have shared their experiences and knowledge in the video interviews used within the module:
• Chris Macey – The Irish Heart Foundation, R.Ireland
• Pnina Rosenzweig – Neeman Association for Stroke Survivors, Israel
• Markus Wagner – Stiftung Deutsche Schlaganfall-Hilfe, Germany
• Monique Lindhout – Hersenletsel, Netherlands
• Jon Barrick – Stroke Alliance for Europe (SAFE)
• Bjørn Magne Bakke – Norsk forening for slagrammede, Norway
Our member and partner organisations who have collaborated in the development of the module content:
• Aivoliitto
• Fundacja Udaru Mózgu
• STROKE-Riksförbundet
• World Stroke Organization
• European Stroke Organisation.
And all those who participated in the User Acceptance Testing of module 3.
We would also like to thank the project sponsor Bayer Healthcare who have supported this project through an education grant.
About SAFE
The Stroke Alliance for Europe (SAFE) a non-profit-making organisation formed in 2004. It is the voice of stroke patients in Europe, representing a range of patient groups from 30 European countries.
SAFE’s goal is to decrease the number of strokes in Europe by advocating for better prevention, access to adequate treatment, post-stroke care and rehabilitation.
For more information about SAFE, please visit www.safestroke.eu

Aug 28, 2018
The original information provided at Braincouncil.eu
In July this year, European Brain Council launched a statement “Counting down to zero: Towards a future with underfunded health research?” which calls on the European Commission, the European Parliament and the Council to increase the budget of the “Horizon Europe” programme to at least €120 billion. What is more, the statement calls on European decision-makers to redistribute the budget in order to ensure that more funding is allocated to the “health” cluster under Pillar II.
The proposal for “Horizon Europe”, published in June 2018, includes an overall budget of €94.1 billion in inflation-adjusted prices. Within this budget, roughly €7.7 billion is proposed to fund the “Health” cluster that is part of the pillar “Global Challenges and Industrial Competitiveness”.
EBC welcomes the increase of the overall draft budget but firmly believes that the proposed budget as it currently stands is insufficient to effectively address today’s societal challenges. The treatment of brain disorders alone is estimated to cost close to €800 billion annually[1], which makes adopting a robust 9th Framework Programme with a strong focus on accelerating health research of paramount importance. What is more, the proposed budget for the “Health” cluster confirms a steady decrease of funding over time and across Framework Programmes, as health was previously allocated 12% under the 7th Framework Programme, 10% under Horizon 2020 and now 8% in the Horizon Europe proposal.
“We are highly concerned about the budget of €7.7 billion provisionally allocated to the “health” cluster under
Pillar II. This amount is not commensurate with the total budget increase and will clearly be insufficient to
effectively address the societal challenges associated with health research. Moreover, this budget confirms a
steady decrease of funding over time and across Framework Programmes, as health was previously allocated
12% under the 7th Framework Programme, 10% under Horizon 2020 and now 8% in the Horizon Europe
proposal. For continued success in European research, we find it imperative that this downward trend is
stopped and reverted.”– says the statement.
The full statement can be accessed here.
EBC invites all organizations, operating at national and/or EU level, that are supportive of the call to join as co-signatory of the statement. Please contact the EBC office (info@braincouncil.eu or +32 (0)2 513 27 57) should you be interested in having the logo of your organization added to the list of signatories.


Aug 8, 2018
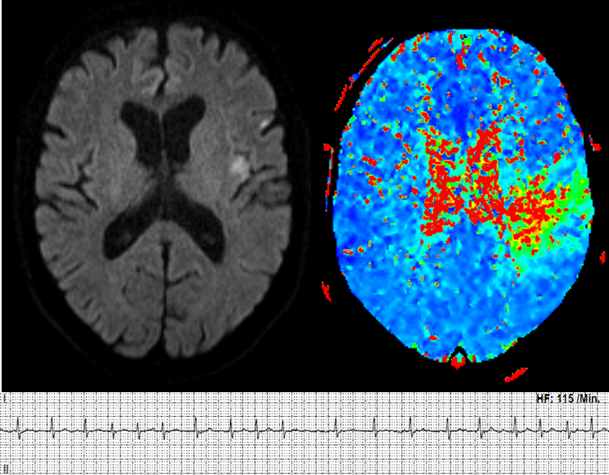
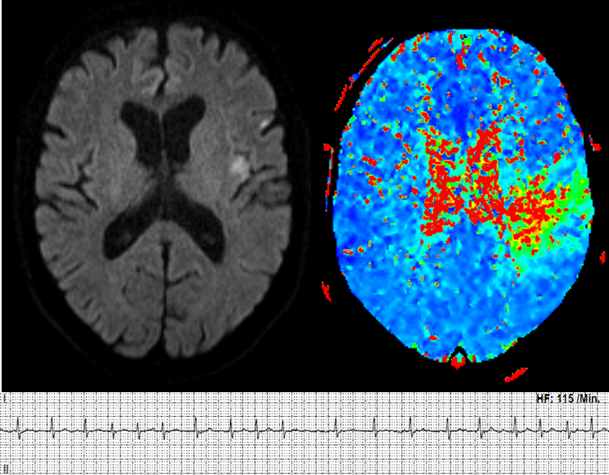
Solitaire™ With the Intention For Thrombectomy Plus Intravenous t-PA Versus DIRECT Solitaire™ Stent-retriever Thrombectomy in Acute Anterior Circulation Stroke (SWIFT DIRECT)
Background
The SWIFT DIRECT trial investigates the emergency treatment of patients with an acute ischaemic stroke. An ischaemic stroke is caused by the blockage of one or more blood vessels in the brain. A clot blocks the blood vessels and blood can no longer circulate. This results in an undersupply of blood and oxygen to the brain regions supplied by these vessels. If the under-supply lasts longer than a few minutes, there is a risk that nerve cells might die. An ischaemic cerebral infarction is a life-threatening situation.
For years, the only causal treatment was the administration of a clot-lysing drug called tissue plasminogen activator. The drug, however, may induce bleedings and is not sufficiently effective in patients with very large clots. In 2014, a new treatment, the so-called mechanical thrombectomy, has been established. With this therapy, nearly all types of large blood clots can directly be removed from the vessel using a specialized catheter. Trials have shown that patients treated with tissue plasminogen activator and mechanical thrombectomy have better outcomes than patients treated with tissue plasminogen activator only. Hence, the current standard treatment in patients with large clots is administration of tissue plasminogen activator followed by mechanical thrombectomy.
As administration of tissue plasminogen activator may also harm the patient and is not effective in patients with large clots, we want to investigate how potent direct mechanical thrombectomy (without prior administration of tissue plasminogen activator) is. The purpose of this trial is thus to compare direct removal of the clot with mechanical thrombectomy versus tissue plasminogen activator administration followed by removal of the clot with mechanical thrombectomy. Only patients with large clots and direct access to mechanical thrombectomy can be included in the trial.
We are conducting this trial to improve the emergency treatment for affected patients with an acute ischaemic stroke. This project is organised by the Neuro Clinical Trial Unit at the University of Bern, Switzerland and will be carried out at several hospitals in Europe and Canada.
What does it mean for patients to participate in this clinical trial?
Trial participants will be assigned by chance to one of two groups (half of the patients will be in each group). In the ‘treatment group’ the blood clot is removed directly with mechanical thrombectomy. In the ‘standard group’, participants first receive blood clot-dissolving medication followed by mechanical thrombectomy to remove the clot.
Both treatment options are commonly used standard treatments. The choice between the two is part of clinical routine at the hospital and lies upon the judgement of the treating physician. Except for the phone interview 90 days after the infarction incident, all examinations are part of standard treatment routine independent from the trial.
General information about the trial
| Study type: |
Multicenter, prospective, randomized, open label, blinded endpoint (PROBE) trial |
| Trial start and end: |
October 2017 to December 2020 |
| Sponsor-Investigators: |
Prof. Dr. med. Urs Fischer, Neurology, and
Prof. Dr. med. Jan Gralla, Neuroradiology,
University Hospital Bern, Inselspital, Switzerland |
| Total number of participants: |
404 patients |
| Trial duration for each participant: |
3 months |
| Participating countries: |
Austria, Canada, Finland, France, Germany, Spain and Switzerland |
| Financial support: |
Medtronic (Minneapolis, USA) |
| Trial registration: |
www.clinicaltrials.gov, No.: NCT03192332 |
Please visit the website www.swift-direct.com for further information.
This trial is endorsed by SAFE.

Aug 8, 2018
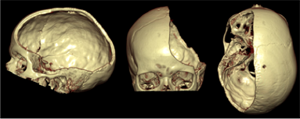
Swiss trial of decompressive craniectomy versus best medical treatment of spontaneous supratentorial intracerebral hemorrhage (SWITCH): a randomized controlled trial
Background
The SWITCH trial investigates the treatment of patients with spontaneous intracerebral hemorrhage (bleeding in the brain). Bleeding in the brain leads to severe brain dysfunctions due to the hemorrhage itself, but also from the brain swelling (brain edema). Each year, about 2 million people worldwide are affected by this disease. The majority of surviving patients remains handicapped. Apart from the standard best medical treatment, there is no possibility to help these patients until now.
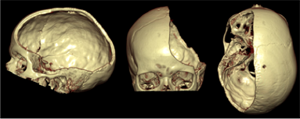 Decompressive craniectomy (removal of parts of the cranial bone) is a standard surgical treatment, which is beneficial in patients with brain swelling after a severe ischemic stroke (under- supply of blood and oxygen in certain brain regions due to occlusion of a blood vessel by a blood clot), after brain injuries, but also in patients with meningitis. However, no trial has so far investigated the effectiveness of decompressive craniectomy in patients with brain bleeding. With this trial we would like to investigate in patients with a brain bleeding, whether this treatment method can reduce mortality and dependency compared to best medical treatment. In a larger context, this trial aims to offer a future treatment option to patients with brain bleeding, which can reduce both mortality and disability.
Decompressive craniectomy (removal of parts of the cranial bone) is a standard surgical treatment, which is beneficial in patients with brain swelling after a severe ischemic stroke (under- supply of blood and oxygen in certain brain regions due to occlusion of a blood vessel by a blood clot), after brain injuries, but also in patients with meningitis. However, no trial has so far investigated the effectiveness of decompressive craniectomy in patients with brain bleeding. With this trial we would like to investigate in patients with a brain bleeding, whether this treatment method can reduce mortality and dependency compared to best medical treatment. In a larger context, this trial aims to offer a future treatment option to patients with brain bleeding, which can reduce both mortality and disability.
This project is organized by the Neuro Clinical Trial Unit at the University of Bern, Switzerland, and is carried out throughout Europe.
What does it mean for patients to participate in this clinical trial?
All patients will be will be assigned by chance to two groups (half of patients will be in each group). In the ‘treatment group’, surgery (decompressive craniectomy) plus best medical treatment will be performed. The patient’s own cranial bone will be re-inserted (re-implanted) after reduction of the swelling in the brain. This usually takes place after about 3 months. In the ‘standard group’, the participants receive best medical treatment, which is the current standard treatment.
A telephone interview will be performed with all patients 30 days, 6 and 12 months after randomization. Apart from the telephone interviews, all examinations are carried out regardless whether or not the patient participates in this trial.
General information about the trial
| Study type: |
Multicenter randomized (1:1) controlled parallel group trial
|
| Trial start and end: |
October 2014 to September 2020
|
| Sponsor-Investigator: |
Prof. Dr. med. Urs Fischer, Inselspital Bern, Switzerland
|
| Participant countries: |
Switzerland, Austria, Germany, Helsinki, Spain, the Netherlands, France
|
| Upcoming participant countries: |
UK
|
| Total Number of participants: |
300 patients |
| Trial duration for each participant: |
12 months |
| Financial support: |
Swiss National Science Foundation (SNCF), Swiss Heart Foundation, Inselspital Foundation |
| Trial registration: |
www.clinicaltrials.gov, No.: NCT02258919 |
For further information, please visit the SWITCH Website
This project is endorsed by SAFE.
Aug 6, 2018
Early versus Late initiation of direct oral Anticoagulants in post-ischaemic stroke patients with atrial fibrillatioN (ELAN) started with the recruitment in October 2017 with currently approximately 80 sites in Switzerland and European countries.
This pragmatic investigator-initiated international trial will add evidence to the best time of starting DOAC after ischaemic stroke in patients with atrial fibrillation. If earlier initiation of DOACs in patients with ischaemic stroke related to atrial fibrillation is shown to be safe and efficacious, this could have a major impact on better treatment adherence, length of hospital stay and patient outcome.
We used an opportunity to talk with Urs Fischer, Professor for Acute Neurology and Stroke (Extraordinarius) at the University Hospital (Inselspital), Bern and principal investigator of the ELAN trial (www.elan-trial.ch).
1. What is ‘atrial fibrillation’ or ‘AF’ and why is it important to know more about it?
Atrial fibrillation is a condition of the heart that is characterized by an abnormal heart rhythm. If you suffer from AF, the atria, two of the chambers in the heart, beat very rapid and irregular. Atrial fibrillation can be episodic or chronic and symptomatic or asymptomatic. It is a very relevant condition because people with atrial fibrillation have a higher risk of suffering from a stroke or a heart failure. Atrial fibrillation is very widespread around the world, especially in the elderly population and causes major mortality and morbidity.
2. What is your personal involvement with the subject of AF, how long are you interested in this subject?
I am currently working as a Professor for Acute Neurology and Stroke at the University Hospital Bern, Switzerland and I am very passionate to find new approaches to prevent and treat strokes. Stroke has a major impact on the quality of life of my patients and their relatives and one of the main causes of a stroke is AF. Therefore, AF needs to be detected and treated.
3. Is there a way to discover AF in time to prevent stroke?
Yes, AF can be detected by cardiac monitoring. Some patients complain about shortness of breath or an irregular pulse. However, it is not uncommon that atrial fibrillation is only diagnosed after the patient has suffered a stroke, especially when AF is asymptomatic and only occurring in episodes and not all the time. Missing these patients is a problem and improving the diagnosis in such patients is a challenge that occupies physicians around the world.
4. Is AF treatable and how?
Atrial fibrillation can be treated or rather managed in a number of ways. The most important approach in the management of AF is to prevent the formation of clots in the heart, which then can cause a stroke or an embolism in other parts of the body. If a patient with AF is at risk of suffering a stroke, anticoagulants (i.e. blood thinners) should be started by the treating physician. If atrial fibrillation is symptomatic by i.e. shortness of breath, cardiologists try to restore a normal heart rhythm. This can be achieved either with drugs or with (minimal invasive) surgery. If the patient is asymptomatic, anticoagulation and frequency control in case of tachycardia are the main goals of therapy.
5. In your opinion, why is the initiation of direct oral Anticoagulants in post-ischaemic stroke patients with atrial fibrillation important?
Post-ischaemic stroke patients are at a high risk of suffering a second stroke soon after the first event. This is called a recurrent stroke. Treatment with oral anticoagulants reduces the risk of a recurrent stroke significantly. Direct oral anticoagulants are the newest class of anticoagulants and compared to older ones, they are just as effective but safer. However, the time point when these drugs should be started after a stroke is unknown. Therefore, we have designed the ELAN trial (Early versus Late initiation of direct oral Anticoagulants in post-ischaemic stroke patients with atrial fibrillatioN (ELAN): an international, multicentre, randomised-controlled, two-arm, assessor-blinded trial; www.elan-trial.ch), in which we currently assess, whether anticoagulants should be started early or with a certain time delay after a stroke.
6. When did the research project ELAN started and what do you expect would change once the research is completed?
The first hospitals started recruiting patients in October 2017. After completion, the results of this trial will help us to understand more about the safety and the potential benefits of an early treatment start with direct oral anticoagulants compared to a later treatment start. The results will give physicians a scientific justification of when to start treatment. ELAN could possibly change the way how post-ischaemic stroke patients with atrial fibrillation are treated.
7. Who is funding this research and do you involve patients/ stroke support organisations in it?
ELAN is funded by the Swiss National Science Foundation and the Swiss heart Foundation. Furthermore, it is endorsed by SAFE, the Stroke Alliance for Europe.
About Prof. Urs Fischer
Urs Fischer is Professor for Acute Neurology and Stroke (Extraordinarius) at the University Hospital (Inselspital), Bern. He is chair of the Neurological Inpatient Department, co-chair of the Stroke Center Bern, and deputy director of the Clinical Trial Unit (CTU) of the University of Bern. He is a clinical researcher and his main research interest involves diagnosis, treatment and outcome of patients with acute neurological diseases. He is co-principal investigator of the SWITCH study (www.switch-trial.ch), principal investigator of the ELAN trial (www.elan-trial.ch) and co-principal investigator of the SWIFT DIRECT trial (www.swift-direct.ch). Urs Fischer is Secretary General of the European Stroke Organisation (ESO), treasurer of the Swiss Neurological Society (SNG) and co-founder the ESO ESMINT ESNR Stroke Winter School, which is regularly held at the University Hospital in Bern, Switzerland.







 Decompressive craniectomy (removal of parts of the cranial bone) is a standard surgical treatment, which is beneficial in patients with brain swelling after a severe ischemic stroke (under- supply of blood and oxygen in certain brain regions due to occlusion of a blood vessel by a blood clot), after brain injuries, but also in patients with meningitis. However, no trial has so far investigated the effectiveness of decompressive craniectomy in patients with brain bleeding. With this trial we would like to investigate in patients with a brain bleeding, whether this treatment method can reduce mortality and dependency compared to best medical treatment. In a larger context, this trial aims to offer a future treatment option to patients with brain bleeding, which can reduce both mortality and disability.
Decompressive craniectomy (removal of parts of the cranial bone) is a standard surgical treatment, which is beneficial in patients with brain swelling after a severe ischemic stroke (under- supply of blood and oxygen in certain brain regions due to occlusion of a blood vessel by a blood clot), after brain injuries, but also in patients with meningitis. However, no trial has so far investigated the effectiveness of decompressive craniectomy in patients with brain bleeding. With this trial we would like to investigate in patients with a brain bleeding, whether this treatment method can reduce mortality and dependency compared to best medical treatment. In a larger context, this trial aims to offer a future treatment option to patients with brain bleeding, which can reduce both mortality and disability.