Dec 20, 2019
First published on ScenceDaily.com
People who take long naps during the day or sleep nine or more hours at night may have an increased risk of stroke, according to a study published in the December 11, 2019, online issue of Neurology®, the medical journal of the American Academy of Neurology.
People who took a regular midday nap lasting more than 90 minutes were 25 percent more likely to later have a stroke than people who took a regular nap lasting from one to 30 minutes. People who took no naps or took naps lasting from 31 minutes to one hour were no more likely to have a stroke than people who took naps lasting from one to 30 minutes.
“More research is needed to understand how taking long naps and sleeping longer hours at night may be tied to an increased risk of stroke, but previous studies have shown that long nappers and sleepers have unfavorable changes in their cholesterol levels and increased waist circumferences, both of which are risk factors for stroke,” said study author Xiaomin Zhang, MD, PhD, of Huazhong University of Science and Technology in Wuhan, China. “In addition, long napping and sleeping may suggest an overall inactive lifestyle, which is also related to increased risk of stroke.”
The study involved 31,750 people in China with an average age of 62. The people did not have any history of stroke or other major health problems at the start of the study. They were followed for an average of six years. During that time, there were 1,557 stroke cases.
The people were asked questions about their sleep and napping habits. Midday napping is common in China, Zhang said. Eight percent of the people took naps lasting more than 90 minutes. And 24 percent said they slept nine or more hours per night.
The study found that people who sleep nine or more hours per night are 23 percent more likely to later have a stroke than people who sleep seven to less than eight hours per night. People who sleep less than seven hours per night or between eight and less than nine hours per night were no more likely to have a stroke than those who slept from seven to less than eight hours per night.
The results were all adjusted for other factors that could affect the risk of stroke. These include high blood pressure, diabetes and smoking.
People who were both long nappers and long sleepers were 85 percent more likely to later have a stroke than people who were moderate sleepers and nappers.
The researchers also asked people about how well they slept. People who said their sleep quality was poor were 29 percent more likely to later have a stroke than people who said their sleep quality was good.
Of the long nappers, 1 percent of cases per person-years later had a stroke, compared to 0.7 percent of cases per person-years of the moderate nappers. The numbers were the same for the long and moderate sleepers, with 1 percent of cases per person-years compared to 0.7 percent of cases per person-years having a stroke.
Read the full article here.
Image: Pixabay

Dec 17, 2019
First published on ScienceDaily.com
A therapeutic shoe engineered to improve stroke recovery is proving successful and expected to hit the market by the end of the year. Clinical trials have been completed on the U.S. patented iStride device, which is licensed by Moterum LLC, a startup company located in the University of South Florida (USF) Research Park. Its results were just published in the Journal of NeuroEngineering and Rehabilitation.
Stroke sufferers experience muscle weakness or partial paralysis on one side of the body, which greatly impacts how they walk, known as gait. Gait asymmetry is associated with poor balance, a major cause of degenerative issues that make individuals more susceptible to falls and injuries.
The iStride device is strapped over the shoe of the good leg and generates a backwards motion, exaggerating the existing step, making it harder to walk while wearing the shoe. The awkward movement strengthens the stroke-impacted leg, allowing gait to become more symmetrical once the shoe is removed. The impaired foot wears a matching shoe that remains stationary.
“The backward motion of the shoe is generated passively by redirecting the wearer’s downward force during stance phase. Since the motion is generated by the wearer’s force, the person is in control, which allows easier adaptation to the motion,” said developer Kyle Reed, PhD, associate professor of mechanical engineering at USF. “Unlike many of the existing gait rehabilitation devices, this device is passive, portable, wearable and does not require any external energy.”
“The importance of over-ground gait training has been emphasized in previous studies,” said Seok Hun Kim, PT, PhD, research collaborator and associate professor in the School of Physical Therapy and Rehabilitation Sciences in the USF Health Morsani College of Medicine. “However, the training options available after stroke are very limited. This novel device allows gait rehabilitation in the environment of daily activities.”
The trial included six people between ages 57 and 74 who suffered a cerebral stroke at least one-year prior to the study. They all had asymmetry large enough to impact their walking ability. Each received twelve, 30-minute gait training sessions for four weeks. With guidance from a physical therapist, the patients’ gait symmetry and functional walking were measured using the ProtoKinetics Zeno Walkway system in the Human Functional Performance Laboratory at USF.
All participants improved their gait’s symmetry and speed. That includes how long it takes to stand up from a sitting position and walk, as well as how long it takes to walk to a specific location and distance traveled within six minutes. Four improved the percentage of time spent in a gait cycle with both feet simultaneously planted on the ground, known as double limb support. As far as the other two that didn’t improve, one started the study with severe impairment, while the other was highly functional. It’s also important to note that three participants joined the study limited to walking in their homes. Following the trial, two of them could successfully navigate public venues.
Read the full article here.
Image: Pixabay

Dec 6, 2019
First published on ScienceDaily.com
The high levels of environmental noise we are subjected to in large cities can increase both the severity and consequences of an ischaemic stroke. More precisely, researchers from the Hospital del Mar Medical Research Institute (IMIM) and doctors from Hospital del Mar, together with researchers from the Barcelona Institute for Global Health (ISGlobal), CIBER in Epidemiology and Public Health (CIBERESP), and Brown University, in the United States, put the increased risk at 30% for people living in noisier areas. In contrast, living close to green areas brings down this risk by up to 25%. This is the first time that these factors have been analysed in relation to stroke severity. The study has been published in the journal Environmental Research.
The researchers looked at the influence of noise levels, air pollution (particularly suspended particles smaller than 2.5 microns; PM2.5), and exposure to green areas on nearly 3,000 ischaemic stroke patients treated at Hospital del Mar between 2005 and 2014. To do this, they used data from the Cartographic Institute of Catalonia, as well as models to analyse atmospheric pollutant levels, the noise map of Barcelona, and satellite images to define areas with vegetation. Also taken into account was the socioeconomic level of the place the patients lived.
Dr. Rosa María Vivanco, from the IMIM’s Neurovascular Research Group and first author of the study, points out that the study gives us initial insight into how noise levels and exposure to green spaces influences the severity of ischaemic stroke. “We have observed a gradient: the more green spaces, the less serious the stroke. And the more noise, the more serious it is. This suggests that factors other than those traditionally associated with stroke may play an independent role in the condition,” she explains. At the same time, Dr. Xavier Basagaña, one of the authors of the study and a researcher at ISGlobal, a centre supported by “la Caixa,” stresses that “exposure to green spaces can benefit human health through various mechanisms. For example, it can reduce stress, encourage social interaction, and increase levels of physical activity.” However, in this study no link was seen with atmospheric pollution. The researchers warn that one of the limitations of the work was the lack of variability in pollutant concentrations to which the study population is exposed. This made it difficult to draw conclusions, and they point out that more studies are needed in this field.
More noise, greater stroke severity
“Previous studies have demonstrated that living in places with high levels of air pollution or noise, or with fewer green areas, exposes the population to a higher risk of suffering an ischaemic stroke. This work broadens our knowledge in this field, showing that the place where we live affects not only the risk of suffering a stroke, but also its severity if it occurs,” explains Dr Gregory A. Wellenius, from the Epidemiology Department at Brown University and final author of the study. In this sense, the results indicate that patients living in noisier areas presented more severe strokes on arrival at hospital.
You can read the full article here.

Dec 5, 2019
First published on ScienceDaily.com
A major UConn School of Medicine study published in the American Heart Association’s flagship journal Circulation shows that more aggressively controlling daily blood pressure in older adults can improve brain health.
It’s been estimated that approximately two-thirds of people over the age of 75 may have damaged small blood vessels in the brain which are visible as bright white lesions on brain imaging. Prior research evidence has linked increased amounts of these white matter lesions in the brain with cognitive decline, limited mobility such as a slower walking speed, increased incidence of falls and even increased stroke risk.
The clinical trial, led by Drs. William B. White of the Calhoun Cardiology Center and Leslie Wolfson of the Department of Neurology, followed 199 hypertension patients 75 years of age and older for 3 years.
Throughout that time, researchers tracked the potential benefits of using an intensive anti-hypertensive medication treatment regimen to garner a 24-hour systolic blood pressure target of less than 130 mmHg compared to standard control (approximately 145 mmHg).
As part of the INFINITY (Intensive Versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline In the Elderly) study, researchers assessed the older adults’ mobility, cognitive function, their brain’s white matter progression with magnetic resonance imaging (MRI), and tracked the occurrence of any adverse events.
While the researchers did not identify any significant differences in cognitive outcomes or walking speed between the two study groups, they did observe a significant reduction in the accumulation of brain white matter disease in those receiving the intensive treatment for blood pressure control.
“The results of INFINITY demonstrate that a lower ambulatory blood pressure goal for older adults is likely to conserve future brain function and health,” said Wolfson, professor of neurology and former chair of the Department of Neurology at UConn Health.
In fact, after three years, the accrual of white matter lesions in the brain were reduced by up to 40% in the those patients receiving the intensive blood pressure therapy compared to those who were on standard therapy.
You can read the full article here.
Dec 3, 2019
First published on ScienceDaily.com
Nagoya City University (NCU) researchers have revealed an interaction between cortico-brainstem pathways during training-induced recovery in stroke model rats, providing valuable insights for improving rehabilitation methods.
Upper limb hemiparesis often occurs after ischemic or hemorrhagic stroke. Unilateral upper extremity impairment can substantially disturb patients’ ability to complete activities of daily living. Therefore, continuous improvement of rehabilitation methods is needed to achieve more positive long-term outcomes among survivors.
Researchers at NCU have identified the dynamic recruitment of the “cortex-to-brainstem” pathways via post-stroke intensive rehabilitation and its contribution to the recovery of impaired forelimb function in intracerebral hemorrhage (ICH) model rats. This crucial finding could provide new insights enabling the improvement of rehabilitative methods for humans.
Stroke often affects the primary network from the cortex to the spinal cord, causing severe ongoing motor deficits. Rehabilitation promotes the recovery of impaired motor function, which is believed to be due to reorganization of the residual neural circuits. However, how the circuits are recruited in rehabilitation-induced recovery remains unclear.
To investigate the mechanisms underlying these phenomena, the NCU team used an ICH rat model in which almost 90% of the cortico-spinal tract is destroyed, causing changes in other motor-related circuits. “We previously found abundant newly formed connections from the motor cortex to the red nucleus in rehabilitated rats,” first author Akimasa Ishida explains. “Interestingly, we also uncovered an increase in the “cortex-to-reticular formation” pathway in trained rats when the “cortico-to-red nucleus” pathway failed to function, using a double-viral infection technique during rehabilitation.”
You can read the full article here.
Nov 15, 2019
PRESS RELEASE ¦ FRIDAY, NOVEMBER 15, 2019 9:00 AM EST
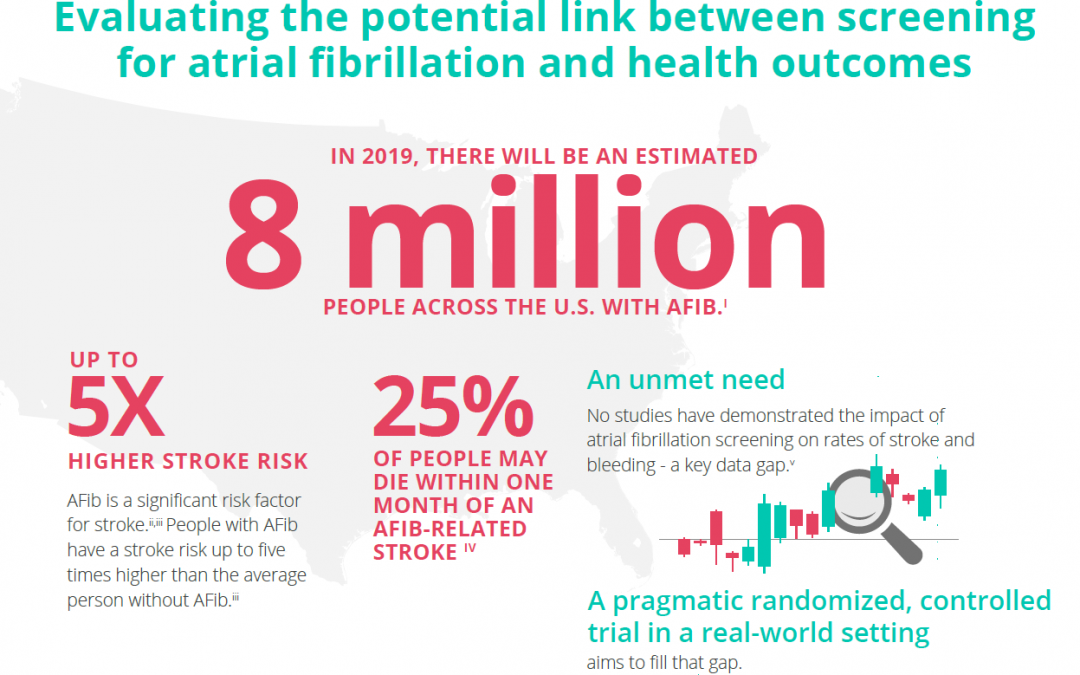
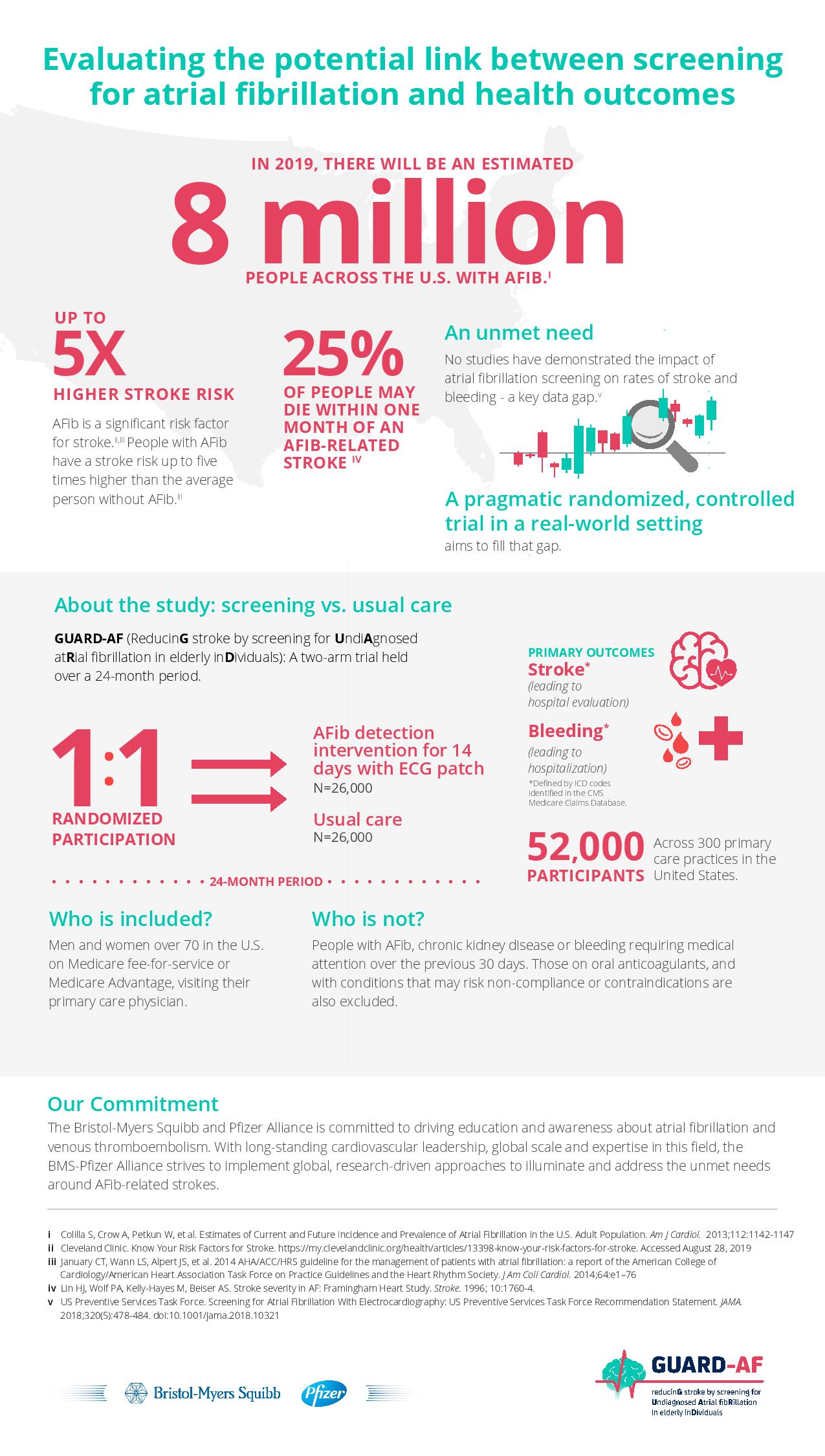
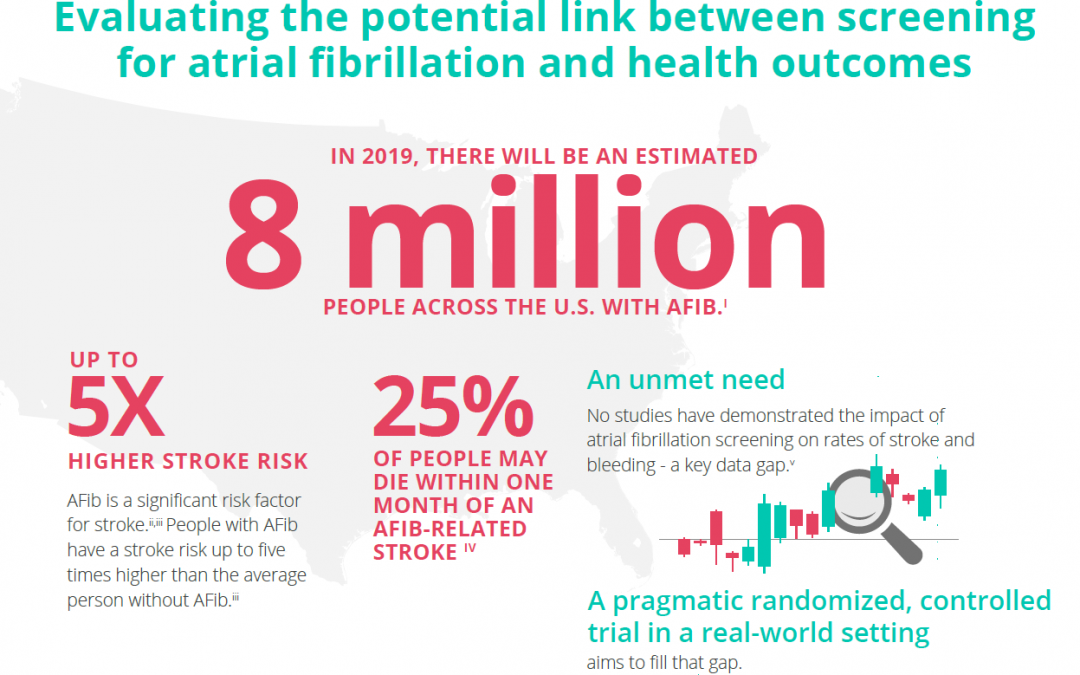
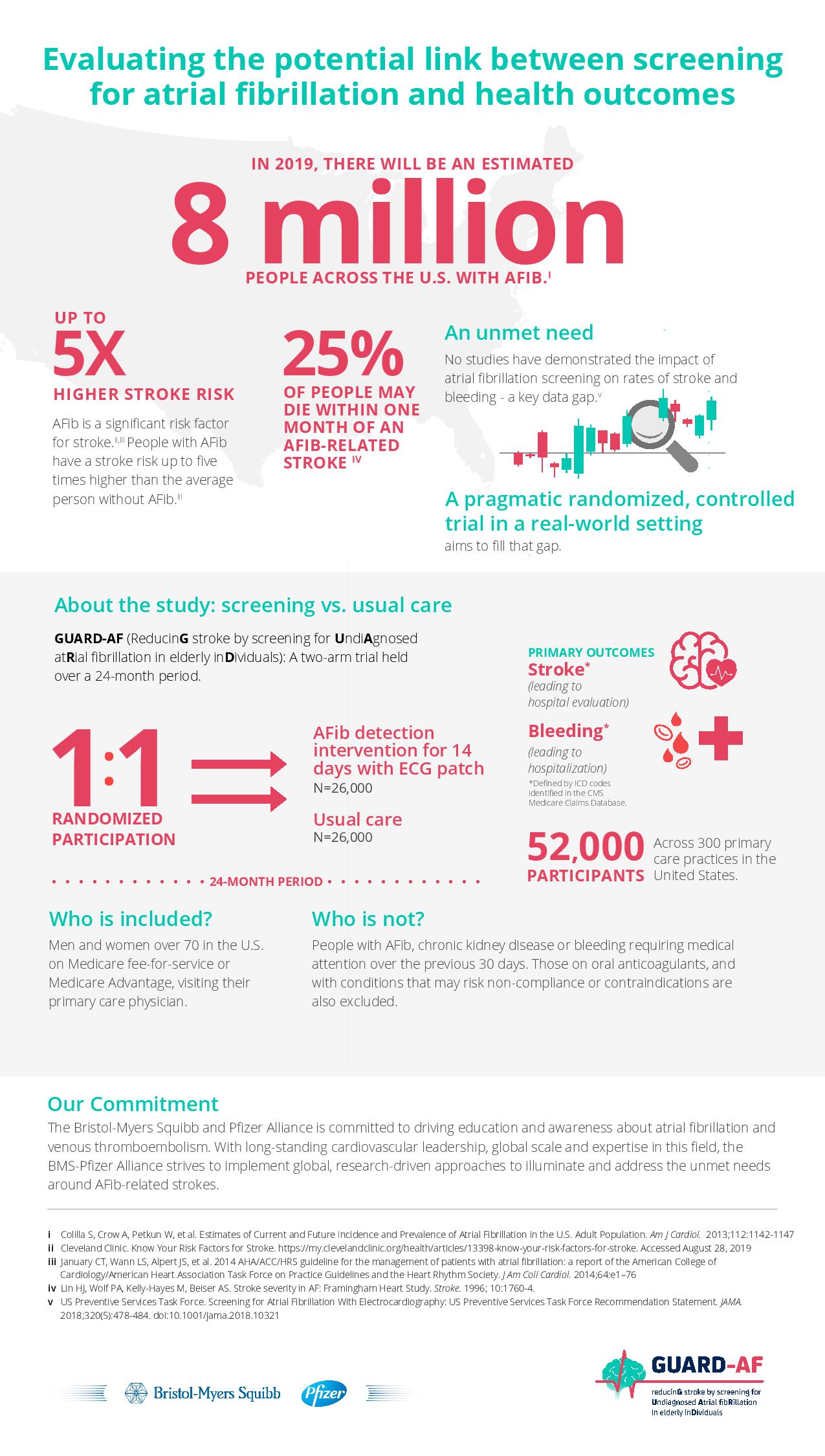
The Bristol-Myers Squibb-Pfizer Alliance today announced the initiation of a new randomized, controlled study, GUARD-AF (ReducinG stroke by screening for UndiAgnosed atRial fibrillation in elderly inDividuals). The study seeks to determine if earlier detection of atrial fibrillation (AFib) through screening in previously undiagnosed men and women at least 70 years of age in the U.S. ultimately impacts the rate of stroke, compared to usual standard medical care. This study will also assess potential bleeding leading to hospitalization, and therefore provide an evaluation of net clinical benefit or harm. AFib is the most common type of significant irregular heart rhythm, and it is estimated that 8 million people in the U.S. will be affected by AFib in 2019.i,ii AFib is a significant risk factor for stroke; stroke risk is up to five times higher in people with AFib than in those without it.iii,iv AFib can often go undetected, as it can be asymptomatic,i and some studies suggest that more than 25 percent of people who have an AFib-related stroke find out they have AFib after a stroke.v
“There is a real need for a study like GUARD-AF to assess the impact of screening for AFib on the crucially important outcome of stroke,” said Daniel Singer, M.D., Professor of Medicine at Harvard Medical School and Professor in the Department of Epidemiology at Harvard T.H. Chan School of Public Health, and an academic general internist at Massachusetts General Hospital. “This study has the potential to directly affect clinical practice and could lead to more AFib patients being identified and appropriately managed to avoid stroke.”
You can read the full press release here.
Disclaimer: This article was written by a third party. It does not necessarily express the views of the Stroke Alliance for Europe. The party who issues this press release is entirely responsible for the accuracy of its information.