
Sep 20, 2018
The original article first published on ScienceDaily.com
One of the largest and longest-running efforts to evaluate the potential benefits of the Mediterranean-style diet in lowering risk of stroke found that the diet may be especially protective in women over 40 regardless of menopausal status or hormone replacement therapy, according to new research in the American Heart Association’s journal Stroke.
Researchers from the Universities of East Anglia, Aberdeen and Cambridge collaborated in this study using key components of a traditional Mediterranean-style diet including high intakes of fish, fruits and nuts, vegetables, cereal foods and potatoes and lower meat and dairy consumption.
Study participants (23,232 white adults, 40 to 77) were from the EPIC-Norfolk study, the United Kingdom Norfolk arm of the multicenter European Prospective Investigation into Cancer study. Over a 17-year period, researchers examined participants’ diets and compared stroke risk among four groups ranked highest to lowest by how closely they adhered to a Mediterranean style diet.
In participants, who most closely followed a Mediterranean-style diet, the reduced onset of stroke was:
- 17 percent in all adults;
- 22 percent in women; and
- 6 percent in men (which researchers said could have been due to chance).
“It is unclear why we found differences between women and men, but it could be that components of the diet may influence men differently than women,” said Ailsa A. Welch, Ph.D., study lead author and professor of nutritional epidemiology at the University of East Anglia, United Kingdom. “We are also aware that different sub-types of stroke may differ between genders. Our study was too small to test for this, but both possibilities deserve further study in the future.”
There was also a 13 percent overall reduced risk of stroke in participants already at high risk of cardiovascular disease across all four groups of the Mediterranean-diet scores. However, this was driven mainly by the associations in women who showed a 20 percent reduced stroke risk. This benefit appeared to be extended to people in low risk group although the possibility of chance finding cannot be ruled out completely.
“Our findings provide clinicians and the public with information regarding the potential benefit of eating a Mediterranean-style diet for stroke prevention, regardless of cardiovascular risk,” said Professor Phyo Myint, M.D., study co-author and former British Association of Stroke Physicians Executive Committee member, University of Aberdeen, Scotland.
“A healthy, balanced diet is important for everyone both young and old,” said Professor Ailsa Welch.
Researchers used seven-day diet diaries, which they said had not been done before in such a large population. Seven-day diaries are more precise than food-frequency questionnaires and participants write down everything they eat and drink over the period of a week.
“The American Heart Association recommends a heart-healthy and brain-healthy dietary pattern that includes a variety of fruits and vegetables, whole grains, low-fat dairy products, fish, poultry, beans, non-tropical vegetable oils and nuts and limits saturated fat, trans fat, sodium, red meat, sweets and sugar-sweetened beverages; this dietary pattern reduces risk factors and risk for heart disease and stroke, “said Eduardo Sanchez, M.D., MPH, the American Heart Association’s chief medical officer for prevention and chief of the Association’s Centers for Health Metrics and Evaluation, who was not a part of this study. “This study provides more evidence that supports AHA’s recommendation,” said Sanchez.
Story Source: American Heart Association. “Mediterranean-style diet may lower women’s stroke risk.” ScienceDaily. ScienceDaily, 20 September 2018. <www.sciencedaily.com/releases/2018/09/180920075854.htm>.
Sep 18, 2018
Conducted by King’s College London on behalf of SAFE in May 2017, the Burden of Stroke Report has now been translated into Greek language. Manuscript translation editing was done by Hariklia Proios, PhD CCC-SLP, Ast. Professor of neurocognitive sciences and rehabilitation, Anna Tsiakiri, PhD Psychologist, Aikaterini Kiriakidou, MD Special Neurologist, Konstantinos Charalampopoulos, MD PhD Special Neurologist and Kalliopi Tsakpounidou, MSc PhD Candidate.
The book will be distributed to the public by the H.N.S.-Hellenic Neurological Society (H.N.S.), the Hellenic Neuropsychological Society (H.NP.S.), the Hellenic Society of Vascular and Endovascular surgery (H.S.V.S.) and the Hellenic (Greek) Stroke Society (Hellenic Society of Cerebrovascular Diseases).
It was presented for the first time in August 31st, 2018, in the board meeting of SAFE in Grand Hotel Palace in Thessaloniki, Greece and will be published by EKDOSEIS GUTENBERG, Printing & Publishing Company – Athens. The aim of the publication is to inform Greek society about the burden of stroke and decrease the rate of this health emergency.

Sep 17, 2018
Reliable, easy to use information on 10 modifiable stroke risk factors all in one place: www.strokeprevention.info
Brussels, 17/09/2018: A SAFE-owned website on stroke prevention and modifiable stroke risk factors goes live today at www.strokeprevention.info.
“We know from the INTERSTROKE study that 10 modifiable risk factors are responsible for 90% of strokes. Our goal is to increase awareness and behaviour change by creating an online resource that will collate all relevant information on the most common risk factors such as: hypertension, physical activity, diet, obesity, smoking, cholesterol, heart disease, alcohol, stress and diabetes.”- said Jon Barrick, the President of SAFE.
This website is a platform which contains all the relevant information on stroke risk factors in an easy and simple format for a range of audiences. All information presented here are in a form appropriate for people with busy lifestyles, unable to digest too much detail at one time, as well as people with disabilities.
Prior to developing this website, our research showed that it was difficult to find consistent and coherent information about stroke prevention in one place online. The problem is that the information is spread across a vast range of different locations: websites, blogs, news portals and e- documents. In addition, many of them are not in a format appropriate for people with disabilities, for example sight impairment.
Note: This website is developed and owned by Stroke Alliance for Europe – SAFE, supported by an educational grant from AMGEN. SAFE retains full editorial control over the content of this website.
About SAFE
The Stroke Alliance for Europe (SAFE) a non-profit-making organisation formed in 2004. It is the voice of stroke patients in Europe, representing a range of patient groups from 30 European countries. SAFE’s goal is to decrease the number of strokes in Europe by advocating for better prevention, access to adequate treatment, post-stroke care and rehabilitation.
For more information about SSOFT and SAFE, please visit www.safestroke.eu.
About Amgen
Amgen is committed to unlocking the potential of biology for patients suffering from serious illnesses by discovering, developing, manufacturing and delivering innovative human therapeutics. This approach begins by using tools like advanced human genetics to unravel the complexities of disease and understand the fundamentals of human biology. Amgen focuses on areas of high unmet medical need and leverages its expertise to strive for solutions that improve health outcomes and dramatically improve people’s lives. A biotechnology pioneer since 1980, Amgen has grown to be one of the world’s leading independent biotechnology companies, has reached millions of patients around the world and is developing a pipeline of medicines with breakaway potential.
In May 2018, Amgen received European Commission approval for Repatha® (evolocumab) to prevent heart attack and stroke in adults with established cardiovascular disease.
For more information, visit www.amgen.com and follow www.twitter.com/amgen.
<End>
Sep 12, 2018
The original article was first published on ScienceDaily.com
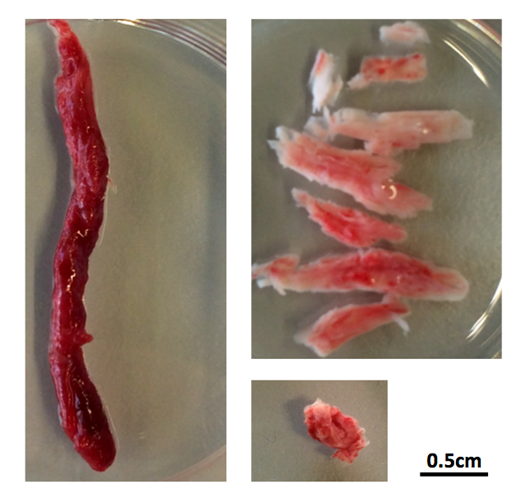
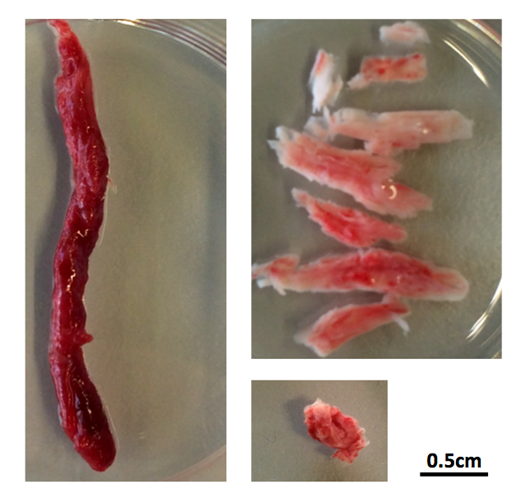
There are two main treatments for stroke caused by a clot in a blood vessel in the brain. One treatment, mechanical thrombectomy, involves pulling the clot out with a specialized catheter that is inserted into the artery in the groin and guided by imaging to the clot. This procedure is only performed at hospitals that specialize in these techniques. The other treatment, which is more widely accessible, involves giving a patient a clot-busting drug that helps the body dissolve the clot.
Quick decision making on which treatment is best for which patient is critical because the clot deprives brain cells of oxygen causing them to die. For physicians, knowing which patients will benefit the most from the clot-buster Alteplase (also known as tPA) just got easier.
University of Calgary scientists with the Hotchkiss Brain Institute at the Cumming School of Medicine (CSM) have discovered that clots have different compositions and depending on where they are located in the brain, administering tPA can be almost as effective as thrombectomy given sufficient time.
“We’ve known that, when administered quickly, tPA can be effective in stroke, but until now, we didn’t realize how effective it can be and we didn’t understand the specific reasons why it works better in some cases than others,” says Dr. Bijoy Menon, MD, associate professor in the departments of Clinical Neurosciences, Radiology and Community Health Sciences at the CSM. “Our findings show that some clots are permeable, which allows the tPA to penetrate the blockage and dissolve it. We saw that within two hours, greater than 50 per cent of permeable blockages had dissolved.”
The UCalgary study led out of the Foothills Medical Centre is the largest of its kind to date, involving nearly 600 patients at 12 medical centres in five countries (Canada, the Czech Republic, South Korea, Spain and Turkey). The findings are published in JAMA.
“Despite earlier research on the benefit of using tPA, we know there is still some reluctance in the medical community to use it. These findings should provide physicians with definitive evidence on the value of giving patients tPA as soon as they’ve confirmed the stroke is due to a clot,” says Dr. Andrew Demchuk, MD, professor in the departments of Clinical Neurosciences and Radiology. “It’s critical that anyone showing symptoms of a stroke be given a CT-angiogram as soon as possible to confirm the blockage. The scan will guide whether tPA is likely to dissolve the clot and may inform whether the patient also needs thrombectomy.”
A CT-angiogram (computer tomography scan) is a common noninvasive diagnostic tool that allows physicians to see images of the blood vessels in the brain. Researchers found that clots in the carotid artery of the brain do not respond to tPA, and for these patients, thrombectomy is required.
“Strokes happen at anytime, anywhere. Knowing who needs thrombectomy can help physicians make better decisions on how to prioritize patient transfers to specialized centres for this procedure,” says Menon. “Data gathered in Europe showed that up to one-third of hospital transfers aren’t necessary.”
“Stroke is an important health care problem and one of the leading causes of death and disability worldwide,” says Dr. Brian H. Rowe, scientific director, Canadian Institutes of Health Research (CIHR) Institute of Circulatory and Respiratory Health, which supported this study. “Through continued scientific research, important discoveries like this one will improve our ability to match patients with the most effective treatment for this particular injury. This will help speed up recovery times, reduce the associated impacts such as paralysis, and it will improve patient outcomes and ultimately save lives.”
Drs. Menon and Demchuk add that for the science community these findings will help researchers better design studies that target dissolving the clot with new clot busting drugs or combination treatments.
Led by the Hotchkiss Brain Institute, Brain and Mental Health is one of six strategic research themes guiding the university towards its Eyes High goals. The strategy provides a unifying direction for brain and mental health research at the university and positions researchers to unlock new discoveries and treatments for brain health in our community.
Story Source: University of Calgary. “Critical differences in clots that cause a stroke: Findings will help inform physicians which treatment will work best for patients.” ScienceDaily. ScienceDaily, 12 September 2018. <www.sciencedaily.com/releases/2018/09/180912081219.htm>.

Sep 12, 2018
The content below was published by Irish Heart Foundation
Irish Heart Foundation launched a “Chairs Can Kill” campaign this week which hoping to help everybody in Ireland sit less and reduce their risk of heart disease and stroke. But why is sitting bad for us?
Recent research has found that sitting for prolonged periods can have a serious effect on our heart health, regardless of whether or not we are exercising [1]. Here comes the science bit: the body needs energy to stand, so to provide this, enzymes in the leg muscles capture fat from the blood to be used for fuel. When you sit for long periods of time the fat is not captured, so it remains in the blood, increasing your risk of heart disease and stroke. Sitting for long periods of time has also been shown to significantly reduce the level of HDL or good cholesterol, in your blood and this too increases your risk of heart disease and stroke [2].
Here are some general tips to help you reduce your sitting time and reduce your risk of heart disease and stroke.
General tips:
Tip 1: Track how long you sit – Do you know just how long you sit for? Use our calculator on irishheart.ie
Tip 2: Set a goal- Try and reduce the amount of time you spend seated. Set a realistic goal.
Tip 3: Break the habit- Why not stand when you can? Be aware of why and when you sit and try to break the habit.
The Irish Heart Foundation has developed a sitting time calculator to help you calculate just how many hours a day you spend sitting down. You can access the calculator here. Also, download our campaign poster and this week’s infographic here to help spread the word.
In addition, why not share the results of your sitting time calculator and see how you can reduce this over the next four weeks of the campaign. Challenge your colleagues to a ‘sit less competition’ and see who manages to reduce their sitting time the most by the end of the campaign. Make sure to let us know how you are reducing your sitting time throughout the month. You can show your support for the campaign by sharing videos and pictures on Facebook, Twitter, Instagram and LinkedIn using #chairscankill.
________________________________________
[1] Biswas et al., 2015 (doi: 10.7326/M14-1651)
[2] Kravitz, L. (2009) (https://www.unm.edu/~lkravitz/Article%20folder/sittingUNM.html)

Sep 10, 2018
Atrial fibrillation (AF) is an abnormal heart rhythm with rapid and irregular beating. It is estimated to increase the risk of stroke 3 to 5-fold and to be associated with around a quarter of all ischaemic strokes. Additionally, AF is associated with more severe strokes leading to higher mortality and disability.
With support from the BMS-Pfizer Alliance, The Economist Intelligence Unit (EIU), London, UK published a new sub-analysis that assessed how 11 EU countries (Belgium, France, Germany, Italy, the Netherlands, Norway, Russia, Spain, Sweden, Turkey and the United Kingdom) compare against European Society of Cardiology’s recommendations for stroke prevention and #AFib detection. This sub-analysis was published in the “Risk Management and Healthcare Policy” journal.
AF is often asymptomatic and screening is not routinely undertaken in Europe. Accurate information on its prevalence in the general population is therefore not widely available. Some European countries have undertaken screening studies to estimate the proportion of the population affected. They reported rates in the general population ranging from 1.3% (UK, Italy) to 3.9% (Greece), with rates being highly dependent on age. Less data is available from Central and Eastern European countries.
Due to Europe’s ageing population and AF’s strong association with age (0.7% in those aged 55-59 vs. 17.8% in those aged ≥85 years), the prevalence of AF is expected to rise. Using data from the community based Rotterdam Study and population projections from Eurostat, it was estimated that the number of adults over 55 with AF will more than double between 2010 and 2060 from 8.8 million to 17.9 million[117]. An Icelandic study projected the prevalence of AF to rise from 1.9% in 2008 to 3.5% in 2050. (Source: Burden of Stroke Report, 2017)
As stated in the Abstract of this sub-study, all 11 participating countries were found to have policies in place to manage general behavioral risk factors of noncommunicable diseases (NCD), but it was found that more needs to be done to address cardiovascular disease – specifically, stroke risk factors. Although ten of the countries in this study endorse the ESC cardiovascular clinical guidelines, implementation is lacking. Eight out of the 11 countries received the lowest score in regard to raising awareness around stroke, and 7 countries were found not to have a stroke registry. Among physicians surveyed in primary care it was reported that less than 30% of patients over 40 years old were screened for blood pressure, whereas even fewer were screened for atrial fibrillation; in 10 out of the 11 countries, less than 20% of patients over 65 years old were screened for atrial fibrillation.
The findings revealed opportunities for improvement in the primary prevention of stroke which should not be ignored, having in mind that the prevalence of AF is expected to rise significantly over the next few decades.

Sep 7, 2018
 Following the publication of EPF’s Transparency Guidelines, European Patients Forum would like to invite you to join a webinar to discuss transparent advocacy in patient organisations.
Following the publication of EPF’s Transparency Guidelines, European Patients Forum would like to invite you to join a webinar to discuss transparent advocacy in patient organisations.
Health advocacy and lobbying is at the heart of the work of many patient organisations (whether it is local, national or European). Their mission statement often includes promoting a political, regulatory, and societal environment that are more patient-centred.
This means that patient organisations engage in lobbying activities on a regular basis. They do so by contributing the specific perspective of patients and people with chronic conditions to legislative processes, but also by pushing for the recognition and for actions on topics that are not yet necessarily on the political agenda (proactive advocacy). Thanks to Vitor Teixeira from Transparency International, the EPF will share with you the benefits of transparency and advocacy as well as a few practical tips on how to enhance your transparency in advocacy activities.
Practical information
Date: Friday 14th September 2018
Time: 15.30-16.15 CEST
How to register?
Register via this link, by 12 September at the latest. Please note that you will need a strong internet connection to fully enjoy the webinar.
And if I can’t make it?
If you can’t make it at the time of the live webinar, no worries! The webinar will be recorded and made available on EPF website.

Sep 4, 2018
The original article first published on ScienceDaily.com
About one third of patients who have suffered a stroke end up with low vision, losing up to half of their visual field. This partial blindness was long considered irreversible, but recent studies have shown that vision training after optic nerve and brain damage can help restore or improve vision. A new study published in the journal Clinical Neurophysiology reports on key mechanisms of vision restoration: attention.
Hemianopia is a decreased vision or blindness in half the visual field, usually as a consequence of stroke or trauma to the brain. It greatly reduces quality of life, affecting patients’ reading, driving and spatial navigation.
“Knowledge in this field is still rather fragmentary, but recent studies have shown that vision can be partially restored by vision training, which improves the deficient visual field sectors,” explains Prof. Bernhard Sabel, PhD, Director of the Institute of Medical Psychology at Magdeburg University, Germany, co-investigator of the study. “Neuroimaging evidence supports a possible role of attention in this vision restoration.”
The study confirmed this hypothesis by obtaining evidence from functional magnetic resonance imaging (fMRI) that visual training led to functional connectivity reorganization of the brain´s attentional network.
Seven chronic hemianopic patients with lesions of the visual cortex took part in vision rehabilitation training for five weeks. After the pre-tests all received training sessions lasting one and a half hours per day for six days per week for five weeks. Each training session, lasting about 60 minutes, was composed of six blocks with 120 training trials each, during which participants had to respond to specially designed visual stimuli on a computer monitor. The pre- and post-test included perimetry testing, contrast sensitivity testing and fMRI scanning one or two days before and after training, respectively. Each contrast sensitivity test consisted of 420 trials in six blocks. The visual rehabilitation training was performed with one eye open, which was randomly chosen, while the non-trained eye was covered with an opaque eye patch.
After training, the patients had significantly improved visual function at the training location, and fMRI showed that the training led to a strengthening of the cortical attentional network connections between the brain region of the right temporoparietal junction (rTPJ) and the insula and the anterior cingulate cortex (ACC).
“Our MRI results highlight the role of attention and the right TPJ activation as a component of vision restoration training in hemianopia,” notes lead investigator Yifeng Zhou, DSc, of the Hefei National Laboratory for Physical Sciences at Microscale and School of Life Science, University of Science and Technology of China, Hefei, P.R. China, and State Key Laboratory of Brain and Cognitive Science, Institute of Biophysics, Chinese Academy of Sciences, Beijing, P.R. China. “However, it is unclear whether the rehabilitation of attentional networks is the direct result of training or the result of the rebalancing of bottom-up sensory streams, which should be investigated in future studies.”
“This discovery that the brain´s attention network is a key mechanism in partially reversing blindness is an exciting advance in the field of restoring vision in the blind, and it opens up new avenues to design new therapies that are even more effective than current methods to help people with low vision or blindness,” concludes Prof. Sabel.
Story Source: Institute for Medical Psychology, Otto-v.-Guericke University Magdeburg. “Attention network plays key role in restoring vision after brain damage: New study highlights the role of attention as a component of vision restoration training in hemianopia.” ScienceDaily. ScienceDaily, 4 September 2018. <www.sciencedaily.com/releases/2018/09/180904114753.htm>.

Sep 3, 2018
The original article published at ScienceDaily.com
People who have had a stroke are around twice as likely to develop dementia, according to the largest study of its kind ever conducted.
The University of Exeter Medical School led the study which analysed data on stroke and dementia risk from 3.2 million people across the world. The link between stroke and dementia persisted even after taking into account other dementia risk factors such as blood pressure, diabetes and cardiovascular disease. Their findings give the strongest evidence to date that having a stroke significantly increases the risk of dementia.
The study builds on previous research which had established the link between stroke and dementia, though had not quantified the degree to which stroke actually increased dementia risk. To better understand the link between the two, researchers analysed 36 studies where participants had a history of stroke, totalling data from 1.9 million people. In addition, they analysed a further 12 studies that looked at whether participants had a recent stroke over the study period, adding a further 1.3 million people. The new research, published in the leading dementia journal Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, is the first meta-analysis in the area.
Dr Ilianna Lourida, of the University of Exeter Medical School, said: “We found that a history of stroke increases dementia risk by around 70%, and recent strokes more than doubled the risk. Given how common both stroke and dementia are, this strong link is an important finding. Improvements in stroke prevention and post-stroke care may therefore play a key role in dementia prevention.”
According to the World Health Organisation, 15 million people have a stroke each year. Meanwhile, around 50 million people globally have dementia – a number expected to almost double ever 20 years, reaching 131 million by 2050.
Stroke characteristics such as the location and extent of brain damage may help to explain variation in dementia risk observed between studies, and there was some suggestion that dementia risk may be higher for men following stroke.
Further research is required to clarify whether factors such as ethnicity and education modify dementia risk following stroke. Most people who have a stroke do not go on to develop dementia, so further research is also needed to establish whether differences in post-stroke care and lifestyle can reduce the risk of dementia further.
Dr David Llewellyn, from the University of Exeter Medical School, concluded: “Around a third of dementia cases are thought to be potentially preventable, though this estimate does not take into account the risk associated with stroke. Our findings indicate that this figure could be even higher, and reinforce the importance of protecting the blood supply to the brain when attempting to reduce the global burden of dementia.”
Story Source: University of Exeter. “Stroke doubles dementia risk, concludes large-scale study.” ScienceDaily. ScienceDaily, 31 August 2018. <www.sciencedaily.com/releases/2018/08/180831083542.htm>.

Aug 31, 2018
Death and illness caused by noncommunicable diseases bring suffering and heartache to millions of people worldwide every year – those who live with the diseases, as well as their families and friends. 70% of all deaths worldwide result from NCDs.
In light of the upcoming Week For Action on NCDs Activities & Comms within the ‘Enough.’ campaign, we used an opportunity to talk with Jelka Jansa, from the Stroke Support Organisation Slovenia. Jelka recently participated in a NCD Alliance workshop in Geneva and being an occupational therapist who works in an acute neurological hospital, she is very familiar with patient support organisations both locally and internationally, especially in the field of stroke.
What is ‘Week For Action on NCDs’ and when is it happening?
It takes place on the 3-9th September. As part of the Enough campaign, the NCD Alliance is encouraging the NCD community all over the world to observe a Global Week of Action on NCDs from the 3rd to 9th of September 2018 in the lead up to the UN HLM on NCDs which will take place later that month on the 27th September. The Global Week for Action on NCDs will catalyse activity among people who are engaged in the NCD movement everywhere, to initiate a transition from commitment to action on NCDs and we encourage you to get involved individually or through your country NCD alliances, in a way that works for you in your context, based on available resources, capacities and priorities.
This will be a global opportunity to talk to each other, to leaders, to media, to crowds, to the world about what works well and what needs to change to ensure a transition from commitment to tangible actions that not only yield reportable improvements in NCD targets and outcomes, but result in the improvement of health and lives of all people in all places.
The opportunities are endless. Possible activities include organising a meeting, street action, picnic, fun run, dance party, art competition or social media support. The week is your chance to do something achievable, appropriate, relevant and impactful where you live, but linked to a global movement. Saying ENOUGH is also a nice way of participating.
Objectives:
-
Show solidarity and a strong united civil society movement to address NCDs globally
-
Draw attention to the UN HLM on NCDs
-
Mobilise around the ENOUGH campaign and emphasise that we all say ENOUGH. Our HEALTH, is our RIGHT, and we need action NOW.
The Global Week for Action will be led by NCD Alliance, with collaborative support of the WHO Civil Society Working Group on NCDs, partners, members, supporters and wider NCD civil society network.
The Guide for Planning your Week for Action on NCDs, Activities and Comms is available for free at this link. It includes useful tips and checklists to help in your planning over the coming three weeks. To complement the guide, you can also find a suite of editable graphics for social media (with English and Spanish versions) to help to promote the Global Week for Action on NCDs and support your activities here.
WHAT HAVE YOU HAD ENOUGH OF?
Share your views and make your own pledge to help stop preventable death and suffering ahead of the 2018 UN HLM on NCDs.
TELL THE WORLD






 Following the publication of EPF’s Transparency Guidelines, European Patients Forum would like to invite you to join a webinar to discuss transparent advocacy in patient organisations.
Following the publication of EPF’s Transparency Guidelines, European Patients Forum would like to invite you to join a webinar to discuss transparent advocacy in patient organisations.





