Feb 11, 2020
Please find below a link to access the new Oruen Round Table. Please be advised that this is for medical professionals.
This is a peer to peer discussion on the role of anticoagulation in the setting of cerebral venous thromboembolism.
- CVT is a rare type of stroke and peripheral venous thromboembolism
- There is scientific evidence supporting anticoagulation in the acute phase of CVT but scant data to guide longer-term oral anticoagulation
- Non-vitamin-K oral anticoagulants (NOACs) are being investigated as an alternative to warfarin in patients with CVT for longer-term management
This discussion’s audience is for the general neurologists and stroke specialists across Europe, once completed, learners will be able to:
- Discuss risk of venous thromboembolism (VTE) after cerebral venous thrombosis (CVT)
- Explain the design of RE-SPECT CVT trial
- Analyse outcomes in RE-SPECT CVT trial
(please note this content is not available for physicians in the UK & US)
Faculty:
José Ferro
Department of Neurosciences and Mental Health
Hospital Santa Maria/Centro Hospitalar Universitário Lisboa Norte
Lisbon, Portugal
Hans-Christoph Diener
Faculty of Medicine
University Duisburg-Essen
Essen, Germany
Jonathan Coutinho
Department of Neurology
Academic Medical Center University of Amsterdam
Amsterdam, The Netherlands
This round table discussion was filmed in Amsterdam by Oruen and was supported by Boehringer Ingelheim.
This discussion has been awarded 1 CME credit by the EACIC; instructions on how to obtain your CME credit will follow at the end of this video.

Feb 7, 2020
Since 2018, SAFE has participated in the Angels Initiative project providing patient perspective and enabling better patient-doctor communication. The project was so far realised in two phases. In the first phase the patient-centered, evidence-based brochures were translated to 13 languages and distributed in 12 countries, in designated stroke hospitals. In the second phase, conducted in late 2019 and early 2020, the project expanded to include even more countries and languages, increasing reach of these information in 15 European countries.
“It’s proven great to have these books and be able to use them as a tool for raising awareness of stroke prevention and treatment among patients, caregivers and people interested in stroke.”
Hrvoje Budinčević
President of the Croatian Stroke Society / Hrvatsko društvo za prevenciju moždanog udara
The brochures were differently formatted, this time being comprised in one booklet containing five types of stroke-related information. SAFE is proud to report that in the second phase 17 out of 34 its stroke support member organisations participated, making these materials available in 14 languages: Spanish, Serbian, Croatian, Catalan, Georgian, Ukrainian, Greek (Greece), Slovakian, Polish, Turkish, Macedonian, Greek (Cyprus), French, Czech and Hungarian.
“International collaboration of SSOs obviously implies exchange of experience and sharing best examples of materials, ideas, projects, etc. From this point preparing of the set of translated and localized education materials on stroke for patients and general population, initially elaborated by one of the leading SSOs in the world, UK Stroke Association, translated to local languages by national SSOs in several countries with support of SAFE and Angels Initiative, is a great experience, showing all of us that we are not alone, and inspiring us for further own efforts.”
Dmitriy Gulyayev
Director of education, research and publishing projects
Ukrainian Anti-Stroke Association
The project was a great success in all countries where it was presented, clearly demonstrating that there was a gap in availability of stroke-related information among patients. Subsequently, it also brought additional quality to doctor-patient communication in hospitals where patients received these books.
The information provided in the books were kindly provided by the Stroke Association UK*and then translated to all project languages, applying the information standard procedure for the translation.
The original brochures are in English language and you can access their original content by following the links below:
Transient ischaemic attack
Next steps after stroke
Supporting a stroke survivor
When you have a stroke
How to reduce your risk
“The Angels project and the brochures are helping us to connect patient voices. I see in it the potential for a possible change in the healthcare system. It means in cooperation with Ministry of Health to set up guidelines which will contain uniform information, for what are patients after stroke entitled in social, physiotherapy or speech therapy sphere.”
Alžbeta Husarovič, President of Porazka.sk
On this link you can find PDF versions in following languages: Greek (for Greece and Cyprus), Hungarian, Czech, Croatian, Serbian, Macedonian, Turkish, Ukrainian, Georgian, Spanish, Catalan, Hungarian, Polish, Slovakian and French.
SAFE Angels Patient Books for Download
To access the last year’s version of books in Latvian language, please click here.
“SAFE Angels books offer consistency of messages, availability of the required information and ability to share this information. Apart from health-related information, they offer plenty of beneficial advices and solutions for obstacles that patients and their caregivers face every day. After using these books for two years, we think they have helped patients to improve their knowledge, compliance to treatment, self-confidence and self management after stroke.”
Maja Bozinovska Smiceska
President of the Macedonian Stroke Association “Mozočen Udar”
SAFE would like to thank and acknowledge support received from our member stroke support organisations who participated in this project:
Serbia: Serbian Stroke Association
Croatia: Croatian Stroke Society
Spain (Catalonia): Fundacio Ictus
Spain: Federacion Espanola de Ictus
Czech Republic: Sdruzeni SMP
Czech Republic: Cerebrum
Georgia: Medical Foundation Mkurnali
Ukraine: Victory over Stroke
Ukraine: Ukrainian Anti-Stroke Association
Hungary: Stroke Liga Nemzeti
Poland: Fundacja Udaru Mozgu
Macedonia: Macedonian Stroke Association “Mozočen Udar”
Greece: HAAS
Turkey: Beyinder
France: France AVC
Slovakia: Porazka.sk
Cyprus: Cyprus Stroke Association
Luxembourg: Bletz ASBL
About the joint SAFE Angels Initiative project
The mission of Boehringer Ingelheim’s (BI’s) Angels Initiative is to increase the number of patients who can be treated in stroke-ready hospitals and to optimise the quality of treatment in all existing stroke centres. The Stroke Alliance for Europe (SAFE) has partnered with BI to support this ambitious project, adding an important dimension: the patient perspective. SAFE’s involvement means patient-focused information will be available to patients and their carers as soon as they arrive in all stroke units.
About Angels Initiative
Every 30 minutes a stroke patient who could have been saved, dies or is permanently disabled, because they were treated in the wrong hospital.
Angels Initiative is building a global community of stroke centres and stroke-ready hospitals, working every day to improve the quality of treatment for every stroke patient.
In 2017, the Angels Initiative was endorsed by European Stroke Organisation (ESO), the largest European organisation of stroke professionals.
For more information about Angels Initiative, please visit www.angels-initiative.com

Feb 6, 2020

Nenad Nikolić, Stroke Association Serbia’s Secretary
Author: Nenad Nikolić, Stroke Association Serbia’s Secretary and Stroke Survivor’s #BrainLifeGoals project manager
During the Brain awareness week, held 11- 17th March 2019, all around the world, many of actions and campaigns took place, aiming to raise public awareness of the progress and benefits of brain research. It was a chance to inform people about the progress in diagnosing, preventing and treating brain disorders. Our Stroke Association Serbia is involved in European and World stroke campaigns, so we used the opportunity to inform our followers about it, using social media and our website.
It was around that time that the European Federation of Neurological Associations launched #BrainLifeGoals campaign. The goal of this campaign is to show and explore aspirations and desires of people who live with brain disorders. Hashtag #Lifegoals has become a popular trend among social media users, clustering their shares about goals and achievements. Sometimes those goals were to have some clothes designed by a famous fashion designer, to earn a lot of money, to travel to exotic destinations, drive a new car… For a person with a brain disorder, these are not important goals- this is luxury, because these people strive for some „basic“ things such as being able to walk again, to read, to write, to talk etc. Things on a daily basis that most of us do automatically and easily can be an achievement and a life goal for someone with brain disorders. We can call them #BrainLifeGoals.
 Our Association recognized the importance of this particular campaign because we could easily relate to it. We decided to support it with active participation. Since I have been managing our Association’s Facebook and Twitter page, and have a very active communication with our followers, I was privileged to receive many people’s stories about their personal experience with stroke.
Our Association recognized the importance of this particular campaign because we could easily relate to it. We decided to support it with active participation. Since I have been managing our Association’s Facebook and Twitter page, and have a very active communication with our followers, I was privileged to receive many people’s stories about their personal experience with stroke.
We decided to publish stories of people with stroke, with an emphasis on their #BrainLifeGoals during their recovery. Than we asked and encouraged those people, most of being in their twenties and early thirties, to share their stories publicly, and to raise awareness of all the problems they’re facing, but also to encourage others with stroke and give them strength to continue their daily struggle with stroke consequences.
No matter how hard we try to advocate for stroke, no one can do it better than someone who has experienced it.
Preparing these stories was a bit of challenge, because there is a lot to be said, and I needed to prioritize. I felt a lot of responsibility, because I was writing about someone’s life, and it had to be done the right way and without many medical terms in order to make understandable for broader audience. The facts and events they told us were shaping stories. Each story was different and had its own concept. All these stories contain variety of emotions: Fear, anxiety, uncertainty, but also hope and huge amount of willpower and support. These stories carry strong messages. Almost every storyteller’s life has changed drastically and these people have now completely different views on life and its aspects, many of them have new hobbies, new healthy habits, many changed their nutrition habits to healthy diets, many of them became more stress tolerant… Highlighting these changes felt like a very important thing to do.

Predrag M. – A middle school physics teacher, a father and a stroke survivor whose #BrainLifeGoal was to be able to read again.
Their #BrainLifeGoals vary from person to person. For someone it was babysitting and playing with their children, for someone cycling, reading, walking without help to nearby sightseeing… Eight stories have been published so far, and some of storytellers had a stroke at the age of 18 and 19! Several more stories are in preparation and will be published soon. Some of our story tellers- Stroke Survivors, had a stroke in their sleep, some while on work. It is clear that stroke can happen anytime, anywhere, to anyone. All these stories have a strong empathetic potential and when read, the reader is faced with situations and problems that the survivors are facing every day. If these stories are encouraging people to think that way, it is our victory! We modified our website www.mozdaniudar.org so every single published story is on one page that can be easily accessed with only one click www.mozdaniudar.org/wp/brainlifegoals/
Except for the important messages stroke survivors tell, it is very important to underline that they also talk openly about stroke. This is, once again, very important, because these wonderful people are encouraging others with stroke to talk freely about their problems, and prevent stigmatization of stroke patients.
The usual procedure is that we first share story on our website and social media accounts, than we translate it to English, and later EFNA shares them on their site www.efna.net/brainlifegoals/ . This way, stories of stroke survivors reach larger international audience. Other Internet portals sometimes share our stories, and we are happy about it. We started with a story of a mother of three who suffered a stroke at 40. Her basic motivation and #BrainLifeGoal was to play again with her children. We continued Campaign with a story of young nursery teacher who had a stroke, and after she recovered, she won a medal in downhill cycling! This inspiring story shows that not only recovery is possible, but also excellent results can be achieved.

Marina K. – A Downhill Biking Champion, a mother and a stroke survivor
In all our cover stories focus is on a stroke survivor, which is very important. For me personally, participating and managing Campaign #BrainLifeGoals in Serbia is a big pleasure, and I really enjoy working on this. I am very proud that our participating in this campaign with working title “Stroke survivor’s brain life goals” is rewarded by EFNA with a grant that really meant a lot to our organisation and helped us organize our core activities.
We are all excited because we feel that we are doing a right thing, helping to raise public awareness about stroke and difficulties that stroke survivors are experiencing in their life after stroke. In a way, we became a “PATIENT VOICE” which is one of our SSO’s basic purposes, and a slogan of the Stroke Alliance for Europe whose member we are proud to be – “The Stroke Patient Voice in Europe”.
Image credits: All images used in this article are property of the Stroke Association Serbia.

Feb 4, 2020
Professor Valeria Caso, Associate Professor of Neurology, University of Perugia Stroke Unit, Perugia, Italy, Professor Helmut Pürerfellner, Department of Cardiology, Public Hospital Elisabethinen, Linz, Austria and Professor Georgios Tsivgoulis, Associate Professor of Neurology, Second Department of Neurology, National & Kapodistrian University of Athens, Greece discussed the different types of stroke and how it is a major healthcare issue. They also discussed the value of prolonged monitoring in selected ESUS patients, and also some new data that might reconfirm what we already know – that if we have longer monitoring in some of those patients, then we will have even better outcomes.
Learning Objectives
- New evidence and increasing the awareness of atrial fibrillation (AF) in cryptogenic stroke patients.
- Treatment approaches from the guidelines and the latest study evidence.
- AF, stroke, and related symptoms, and why the evidence from the past is important.
- Why ESUS needs prolonged monitoring and how new data may benefit patients.
For accessing the webinar video, please click on the button below:
Oruen Webinar
For further information please visit Oruen website.
This webinar was supported by Medtronic.

Jan 31, 2020
First published on ScenceDaily.com
New research from the Smidt Heart Institute at Cedars-Sinai showed for the first time that women’s blood vessels — including both large and small arteries — age at a faster rate than men’s. The findings, published Wednesday in the journal JAMA Cardiology, could help to explain why women tend to develop different types of cardiovascular disease and with different timing than men.
“Many of us in medicine have long believed that women simply ‘catch up’ to men in terms of their cardiovascular risk,” said Susan Cheng, MD, MPH, MMSc, senior author of the study and director of Public Health Research at the Smidt Heart Institute. “Our research not only confirms that women have different biology and physiology than their male counterparts, but also illustrates why it is that women may be more susceptible to developing certain types of cardiovascular disease and at different points in life.”
Using community-based data amassed from multiple sites across the country, Cheng and her research team conducted sex-specific analyses of measured blood pressure — a critical indicator of cardiovascular risk. The data represented nearly 145,000 blood pressure measurements, collected serially over a 43-year period, from 32,833 study participants ranging in age from 5 to 98 years old.
Because a person’s risk for developing a heart attack, heart failure, or a stroke typically begins with having high blood pressure, Cedars-Sinai researchers combed through their massive data looking for clues and patterns regarding how blood pressure starts to rise. Then, instead of comparing the data from men and women to each other, investigators compared women to women and men to men.
This approach allowed investigators to identify that the progression and evolution of women’s vascular function is very different than for men. In fact, women showed signs of blood pressure elevation much earlier in life than men.
“Our data showed that rates of accelerating blood pressure elevation were significantly higher in women than men, starting earlier in life,” said Cheng, the Erika J. Glazer Chair in Women’s Cardiovascular Health, who also serves as director of Cardiovascular Population Sciences at the Barbra Streisand Women’s Heart Center. “This means that if we define the hypertension threshold the exact same way, a 30-year old woman with high blood pressure is probably at higher risk for cardiovascular disease than a man with high blood pressure at the same age.”
Christine Albert, MD, MPH, founding chair of the newly established Department of Cardiology at the Smidt Heart Institute, says this new research should help guide clinicians and researchers to think differently when it comes to treating and studying women and their cardiovascular health.
You can read the full article here.
Image: Pixabay

Jan 24, 2020
First published on ScienceDaily.com
It’s been almost a quarter century since the first drug was approved for stroke. But what’s even more striking is that only a single drug remains approved today.
In a publication appearing this month in the journal Translational Stroke Research, animal scientists, funded by the National Institutes of Health, present brain-imaging data for a new stroke treatment that supported full recovery in swine, modeled with the same pattern of neurodegeneration as seen in humans with severe stroke.
“It was eye opening and unexpected that you would see such a benefit after having had such a severe stroke,” said Steven Stice, Georgia Research Alliance Eminent Scholar and D.W. Brooks Distinguished Professor in the University of Georgia’s College of Agricultural and Environmental Sciences. “Perhaps the most formidable discovery was that one could recover and do so well after the exosome treatment.”
Stice and his colleagues at UGA’s Regenerative Bioscience Center report the first observational evidence during a midline shift — when the brain is being pushed to one side — to suggest that a minimally invasive and non-operative exosome treatment can now influence the repair and damage that follow a severe stroke.
Exosomes are considered to be powerful mediators of long-distance cell-to-cell communication that can change the behavior of tumor and neighboring cells. The results of the study echo findings from other recent RBC studies using the same licensed exosome technology.
Many patients who suffer stroke exhibit a shift of the brain past its center line — the valley between the left and right part of the brain. Lesions or tumors will induce pressure or inflammation in the brain, causing what typically appears as a straight line to shift.
“Based on results of the exosome treatment in swine, it doesn’t look like lesion volume or the effects of a midline shift matter nearly as much as one would think,” said Franklin West, associate professor of animal and dairy science in the UGA College of Agricultural and Environmental Sciences. “This suggests that, even in some extremely severe cases caused by stroke, you’re still going to recover just as well.”
You can read the full article here.
Image: Pixabay

Jan 24, 2020
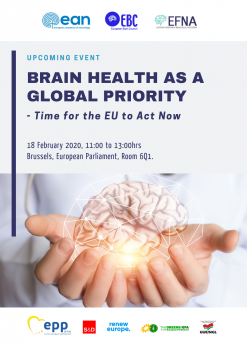
First published on EFNA website – Event announcement and invitation
On 18 February 2020, EFNA together with EBC and EAN, will hold the event “Brain Health as a Global Priority – Time for the EU to Act Now” in the European Parliament, Brussels from 11am to 1pm in Room 6Q1, hosted by Jarosław Duda, EPP.
Follow this link to register via EFNA website.
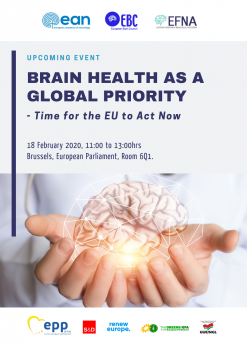 The event is held under the patronage of Members of the European Parliament [EP]:
The event is held under the patronage of Members of the European Parliament [EP]:
- Ewa Kopacz, Vice President of the EP, European People’s Party [EPP]
- Mairead McGuinness, Vice President of the EP, European People’s Party [EPP]
- Miriam Dalli, Vice-Chair, Group of the Progressive Alliance of Socialists and Democrats [S&D]
- Frédérique Ries, Vice-Chair, Renew Europe [RE]
- Kateřina Konečná, European United Left–Nordic Green Left [GUE/NGL]
- Tilly Metz, Group of the Greens/European Free Alliance [EFA]
The event looks to explore the following:
Is brain health a global priority?
In the Political Declaration on Non-Communicable Diseases (NCDs), which arose from the United Nations (UN) High-Level Meeting on NCDs in 2018, all Governments recognized that ‘mental disorders and other mental health conditions, as well as neurological disorders, contribute to the global burden of NCDs. It resulted in adding mental and neurological health as the ‘5th NCD’, complementing global efforts to combat cancer, CVD, diabetes and chronic respiratory diseases. This has been reinforced in the recent 2019 UN Declaration on the Universal Health Coverage, where ‘mental disorders and other mental health conditions as well as neurological disorders’ have been identified as an ‘essential component of UHC’. Additionally, the World Health Organisation (WHO) is also now building a new Brain Health team to operate from its headquarters in Geneva. The question now is how can we ensure this progress can be translated into policy action at EU and member state level?
You can access more information and agenda by following this link.

Jan 15, 2020
We are delighted to share with you a report from the German Stroke Foundation about their key activities between July and December 2019. We hope it will inspire you and your organisation for activities in your country.
World stroke day: “Every step counts”

Miriam_Mashkoori, World Stroke Day 2019
Statistically 25 percent of the worlds population gets a stroke. This also means: 3 out of 4 people do not get a stoke!
Around World Stroke Day (October 29th) the German Stroke Foundation raised awareness for stroke-prevention with the slogan “every step counts”. Many papers published the press release with tips for a healthier lifestyle, radio-stations aired an interview with the foundations prevention-expert Miriam Mashkoori. On Facebook people explained how they lost weight or managed to quit smoking to motivate other Facebook-users to live a healthier life.
Summer Camp for children and their families
 How will my child develop? How will it do in Kindergarten or school? How do we cope with social challenges and which therapies are best with for our child? The diagnosis “stroke” raises many questions – especially when a child is affected. The three day “Summer Camp” offered families with a child affected by stroke an opportunity for an informative and fun-filled weekend. Experts answered questions, psychologists helped developing new perspectives, singer Patricia Kelly gave an exclusive concert and former world-class Wrestler Alexander Leipold offered sport-activities for the children.
How will my child develop? How will it do in Kindergarten or school? How do we cope with social challenges and which therapies are best with for our child? The diagnosis “stroke” raises many questions – especially when a child is affected. The three day “Summer Camp” offered families with a child affected by stroke an opportunity for an informative and fun-filled weekend. Experts answered questions, psychologists helped developing new perspectives, singer Patricia Kelly gave an exclusive concert and former world-class Wrestler Alexander Leipold offered sport-activities for the children.
Tea Time with Liz Mohn
The foundation´s president and founder Liz Mohn invited stroke survivors and supporters of the foundation for a Tea Time. She met and spent a wonderful afternoon with people who were especially engaged in our foundation´s activities.
Workshop for young stroke-survivors
 A stroke affects every aspect of life. Young survivors are even in a special situation. They want to return to work, build or maintain relationships and live an independent life – which is not always possible. In a four-day workshop they had the opportunity to talk to psychologists and doctors and to exchange their own experiences. Word-class Mountainbiker Peter Schermann talked about his return into sports after his stroke.
A stroke affects every aspect of life. Young survivors are even in a special situation. They want to return to work, build or maintain relationships and live an independent life – which is not always possible. In a four-day workshop they had the opportunity to talk to psychologists and doctors and to exchange their own experiences. Word-class Mountainbiker Peter Schermann talked about his return into sports after his stroke.
Public talk about reintegration in working life

After an accident or an illness it is often hard to return to work. Some might not be able to work full hours anymore, others might have to find a completely different job. A staff member of the employment office, an integration expert and a coach for job applications informed about opportunities to get back to work at the event “Forum Schlaganfall (Stroke Forum)” at the German Stroke Foundation in Gütersloh.
Politican Andrea Milz visits the Stroke Foundation

Andrea Milz
The North Rhine Westphalian secretary of state for sports and volunteering, Andrea Milz, visited the German Stroke Foundation to talk about the volunteer-project “stroke helpers”.
As a certified Zumba-trainer she also gave a Zumba-lesson at the local High School. The High School offers optional medicine-classes for its students and cooperates with the foundation.
Speakers of self support groups meet
Speakers of self support groups do not only organise meetings and events for their groups. But they also need to know about relevant changes in law, new therapies or other important aspects about stroke. This is why the foundation offers workshops for speakers of self support groups all over Germany.

Cooperation with TV-show “Unter uns” ends

Patrick Müller
One of the main characters in the popular TV series “Unter uns” has had a stroke in one of the episodes in May. According to the storyboard lawyer Tobias, played by actor Patrick Müller, suffered from hemiplegia and severe speech problems. The team and cast of “Unter uns” cooperated with the German Stroke Foundation in order to create a realistic storyline. The cooperation know officially ended. The fan-club donated more than 1400 Euros for the foundation.
Experts meet to learn about stroke in children
 Not many people know that children can have a stroke. Even experts like podiatrists or therapists often don’t have sufficient information about the topic. The German Stroke Foundation wants to change this by inviting experts to learn more about child stroke. More than 40 doctors and other experts met in Bavaria in 2019.
Not many people know that children can have a stroke. Even experts like podiatrists or therapists often don’t have sufficient information about the topic. The German Stroke Foundation wants to change this by inviting experts to learn more about child stroke. More than 40 doctors and other experts met in Bavaria in 2019.
Photos: German Stroke Foundation, 2019

Jan 10, 2020
First published on ScienceDaily.com
Middle-aged adults with high blood pressure, Type 2 diabetes, heart disease or stroke could be at high risk for cancer and early death when sleeping less than six hours per day, according to new research published in the Journal of the American Heart Association, the open access journal of the American Heart Association.
“Our study suggests that achieving normal sleep may be protective for some people with these health conditions and risks,” said lead study author Julio Fernandez-Mendoza, Ph.D., associate professor at Pennsylvania State College of Medicine and sleep psychologist at the Sleep Research & Treatment Center of the Penn State Health Milton S. Hershey Medical Center in Hershey, Pennsylvania. “However, further research is needed to examine whether improving and increasing sleep through medical or behavioral therapies can reduce risk of early death.”
Researchers analyzed data of more than 1,600 adults (20 to 74 years old, more than half women) from the Penn State Adult Cohort who were categorized into two groups as having stage 2 high blood pressure or Type 2 diabetes and having heart disease or stroke. Participants were studied in the sleep laboratory (1991-1998) for one night and then researchers tracked their cause of death up to the end of 2016.
Researchers found:
Of the 512 people who passed away, one-third died of heart disease or stroke and one-fourth died due to cancer.
People who had high blood pressure or diabetes and slept less than 6 hours had twice the increased risk of dying from heart disease or stroke.
People who had heart disease or stroke and slept less than 6 hours had three times the increased risk of dying from cancer.
The increased risk of early death for people with high blood pressure or diabetes was negligible if they slept for more than 6 hours.
You can read the full article here.
Image: Pixabay.com
Jan 7, 2020
First published on ScienceDaily.com
A team of New Jersey stroke researchers has linked recovery of reading and language competence with cerebral blood flow in the left reading network. Their findings may contribute to new approaches to identifying and treating reading deficits after stroke. The open access article, “Cerebral perfusion of the left reading network predicts recovery of reading in subacute to chronic stroke” was epublished on August 26, 2019 in Human Brain Mapping. The authors are Olga Boukrina, PhD, and A.M. Barrett, MD, of Kessler Foundation, and William Graves, PhD, of Rutgers, the State University of New Jersey.
Despite the fundamental role of reading ability in everyday living, little research has been conducted on patterns of reading recovery after stroke, or the development of interventions to improve reading outcomes. In this study of left-brain stroke, a team of New Jersey scientists examined patterns of cerebral perfusion bilaterally, including left and right networks of brain areas important for healthy reading, the area surrounding the stroke lesion, and the corresponding contralateral area.
They enrolled 31 participants during inpatient rehabilitation, within 5 weeks of left-sided stroke. All underwent functional magnetic resonance imaging, psychometric testing, neurological examination and tests for phonological, orthographic and semantic impairments. Fifteen participants had follow-up studies at 3 months post stroke. Analysis of data from the subacute and chronic phases showed that recovery of reading and language competence correlated with increases in cerebral blood flow in the left reading network.
You can read the full article here.
Image: Pixabay.com






 Our Association recognized the importance of this particular campaign because we could easily relate to it. We decided to support it with active participation. Since I have been managing our Association’s Facebook and Twitter page, and have a very active communication with our followers, I was privileged to receive many people’s stories about their personal experience with stroke.
Our Association recognized the importance of this particular campaign because we could easily relate to it. We decided to support it with active participation. Since I have been managing our Association’s Facebook and Twitter page, and have a very active communication with our followers, I was privileged to receive many people’s stories about their personal experience with stroke.





 The event is held under the patronage of Members of the European Parliament [EP]:
The event is held under the patronage of Members of the European Parliament [EP]:

 How will my child develop? How will it do in Kindergarten or school? How do we cope with social challenges and which therapies are best with for our child? The diagnosis “stroke” raises many questions – especially when a child is affected. The three day “Summer Camp” offered families with a child affected by stroke an opportunity for an informative and fun-filled weekend. Experts answered questions, psychologists helped developing new perspectives, singer Patricia Kelly gave an exclusive concert and former world-class Wrestler Alexander Leipold offered sport-activities for the children.
How will my child develop? How will it do in Kindergarten or school? How do we cope with social challenges and which therapies are best with for our child? The diagnosis “stroke” raises many questions – especially when a child is affected. The three day “Summer Camp” offered families with a child affected by stroke an opportunity for an informative and fun-filled weekend. Experts answered questions, psychologists helped developing new perspectives, singer Patricia Kelly gave an exclusive concert and former world-class Wrestler Alexander Leipold offered sport-activities for the children. A stroke affects every aspect of life. Young survivors are even in a special situation. They want to return to work, build or maintain relationships and live an independent life – which is not always possible. In a four-day workshop they had the opportunity to talk to psychologists and doctors and to exchange their own experiences. Word-class Mountainbiker Peter Schermann talked about his return into sports after his stroke.
A stroke affects every aspect of life. Young survivors are even in a special situation. They want to return to work, build or maintain relationships and live an independent life – which is not always possible. In a four-day workshop they had the opportunity to talk to psychologists and doctors and to exchange their own experiences. Word-class Mountainbiker Peter Schermann talked about his return into sports after his stroke.



 Not many people know that children can have a stroke. Even experts like podiatrists or therapists often don’t have sufficient information about the topic. The German Stroke Foundation wants to change this by inviting experts to learn more about child stroke. More than 40 doctors and other experts met in Bavaria in 2019.
Not many people know that children can have a stroke. Even experts like podiatrists or therapists often don’t have sufficient information about the topic. The German Stroke Foundation wants to change this by inviting experts to learn more about child stroke. More than 40 doctors and other experts met in Bavaria in 2019.