Nov 29, 2019
„This year’s Working Conference was a little different compared to others, because every single delegate who registered actually came to the conference“, said Jon Barrick, SAFE President in his opening remarks of the most important SAFE annual event.
More than 80 delegates from over 30 European countries gathered in Porto, Portugal for this year’s conference and General Assembly.
The Working Conference agenda covered important topics ranging from SAFE’s advocacy work and workshops about growing a stroke support organisation, to vitally important day-to-day topics such as stroke and intimacy, fatigue after stroke and travelling if you are a stroke survivor.
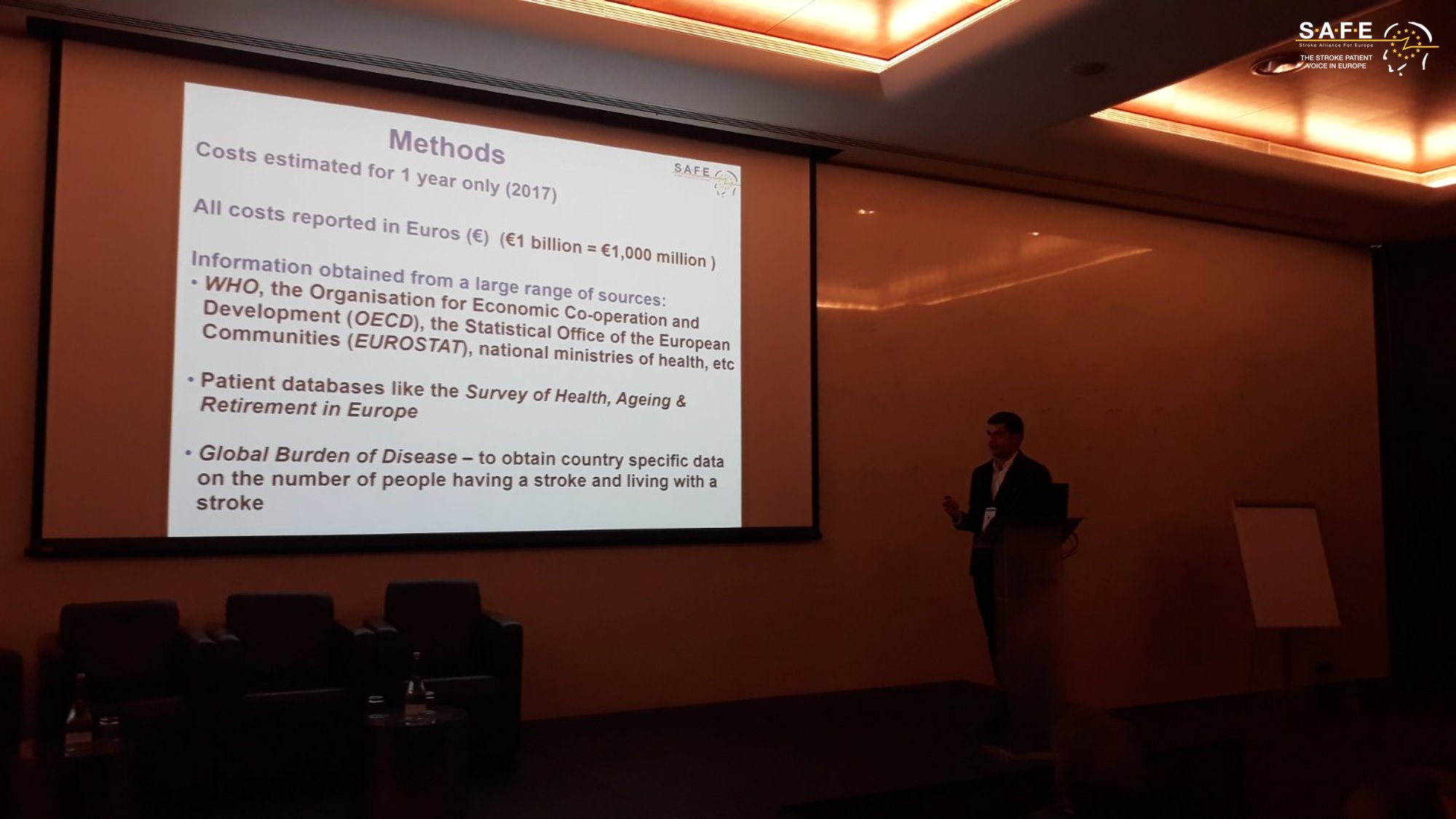
On the first day of the Working Conference SAFE’s most important project in 2019 was presented – The Economic Impact of Stroke in Europe Report.This pivotal piece of research into the health economics of stroke in Europe was presented by Ramon Luengo Fernandes, research lead on behalf of the University of Oxford and Gary Randall, SAFE’s Research Manager and volunteer.
“The Economic Impact of Stroke in Europe Report provides persuasive arguments for stroke to be considered as an investable proposition. We hope we have brought enough hard evidence for our partners, medics, researchers and policy decision makers to see the clear potential for investment in stroke prevention, treatment and life after stroke as a way for saving more lives and reducing future costs” said Arlene Wilkie, SAFE Director General and the chair of this session.
The whole session with the presentation of the results was live tweeted and shared via SAFE Facebook page.
You can see the agenda of the SAFE Working Conference here.
The second day was about practical information on how to grow an SSO, presented by Sarah Belson from the World Stroke Organisation. ‘How to develop your organisation’ is of course a huge topic, but having spoken to a number of you I recognise that some of the most valuable learning you take from SAFE, is hearing from the experience of other SSOs” said Sarah Belson. She presented four case studies from the Cyprus, Finland, Poland and Israel SSOs.
SAFE’s General Assembly was held on 29th November. Apart from voting for very important updates in the SAFE Constitution, new members were welcomed to the Board and three new organisations joined SAFE- Moždani Val from Croatia, Ukrainian Anti-Stroke Association and Turkish Cerebrovascular Diseases Society. The SAFE Assembly voted with much regret for the expulsion of the Austrian SSO, as this member failed to fulfill its membership duties.
There were three new candidates for the Board and three candidates from the previous Board were standing for re-election. After expressing unanimous decisions for each candidate, delegates’ vote lead to SAFE having the full Board in 2020. The new Board consists of 11 members:
Jon Barrick, SAFE President, UK
Anita Arsovska, Vice President, North Macedonia
Marina Charalambous, Secretary, Cyprus
Chris Macey, Treasurer, Ireland
Grethe Lunde, Norway
Ivan Milojević, Serbia
Derya Uluduz, Turkey
Dmytro Gulyayev, Ukraine
Hrvoje Jurlina, Croatia,
Hariklia Proios, Greece
Pnina Rosenzweig, Israel

After 15 amazing years of serving #SAFE, Markus Wagner from the German Stroke Foundation Stiftung Deutsche Schlaganfall-Hilfe was presented with a token of our appreciation for all of his hard work as a SAFE Board member, Past-President and a VP. We really appreciate Markus as a colleague and a friend and we hope he will continue to share his experience and ideas with SAFE.
The next General Assembly will be held on 20th November 2020 in Barcelona, Spain.

Nov 27, 2019
In 2017, nearly 1.5 million people suffered a stroke, nine million Europeans lived with a stroke, and more than 430,000 people died due to a stroke in the 32 countries in a new study. The total annual costs for stroke were over €60 billion, a figure revealed by the Economic Impact of Stroke in Europe Report, funded by the Stroke Alliance for Europe (SAFE) and undertaken by a health economics team from the University of Oxford.
“We know stroke shatters lives. This latest evidence clearly demonstrates its ability to shatter entire economic systems if the business as usual approach continues” said Arlene Wilkie, SAFE Director General confirming the first part of the Economic Impact of Stroke in Europe report being published in the European Stroke Journal.
SAFE delegates at the Working Conference held in Porto today had an exclusive opportunity to hear first-hand about this research and its most important findings from Ramon Luengo Fernandes, research lead on behalf of the University of Oxford and Gary Randall, SAFE’s Research Manager and volunteer.
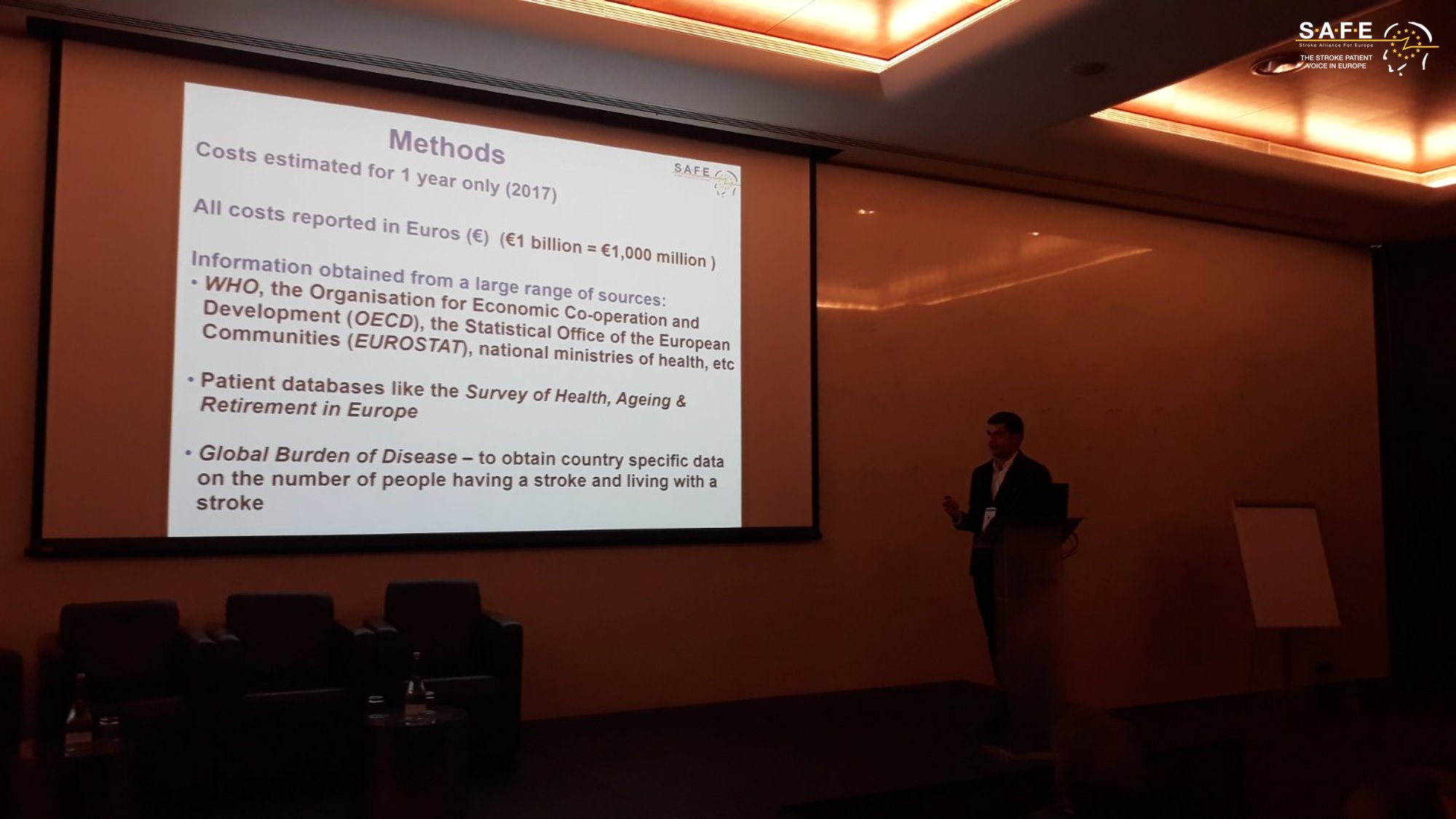
Ramon Luengo Fernandes, University of Oxford
The whole session with the presentation of the results was live tweeted and shared via SAFE Facebook.
Previously, in 2015, the overall cost of stroke for the European Union was estimated to be €45 billion. However, that study did not include nursing or residential care home costs, which may have biased the estimated costs of stroke downwards because evidence has shown that when a stroke happens, the survivor often needs to be placed in a specialised institution for further care, for example in a nursing home.

Gary Randall, SAFE Research Manager
This new study shows that with social care costs (nursing and residential care home costs), costs of productivity losses (the effect of sickness on person’s time off work; working years lost due to early death) and informal care costs (the time that relatives and friends spend providing unpaid care to people with stroke) being added, we have the first full overview of all stroke-related costs in all 32 countries in question. With this new information, the cost of stroke across 32 European countries is roughly 15 billion euros more than previously estimated in 2015. However, this is likely to be an underestimate, because some categories of healthcare costs, such as health education, public health activities, supportive treatments, home adaptations, and care provided outside the healthcare system were not recorded in healthcare statistics.
Further work commissioned by SAFE will estimate the number of people having, living and dying from stroke in 2030, 2035 and 2040, and how these changes will impact the economic costs of stroke across the 32 European countries in the study. These findings will be revealed in May 2020.
“The Economic Impact in Europe Report provides persuasive arguments for stroke to be considered as an investable proposition. We hope we have brought enough hard evidence for our partners, medics, researchers and policy decision makers to see the clear potential for investment in stroke prevention, treatment and life after stroke as a way for saving more lives and reducing future costs” concluded Arlene Wilkie.
This Report was made possible through educational grants from the following organisations: Boehringer Ingelheim, Amgen, Allm and the BMS-Pfizer Alliance.

Nov 22, 2019
Press Release | Source: EFNA
Launched in 2019, the #BrainLifeGoals campaign is raising awareness of the impact of neurological disorders by exploring the dreams and aspirations of those affected.
Sharing #LifeGoals has become a popular trend in social media. #LifeGoals are the often frivolous wishes people have – for example to own a designer handbag, meet a film star or drive a Maserati! Through this campaign people are putting a new spin on the trend by instead sharing their #BrainLifeGoals.
The campaign is an initiative of the European Federation of Neurological Associations (EFNA), an umbrella organisation representing pan-European neurology patient groups.
What are your #BrainLifeGoals for the New Year?
We’re approaching New Year- a time when it is traditional in many parts of the world to resolve to makes changes for the better, or to accomplish a personal goal. As part of the #BrainLifeGoals campaign EFNA is pleased to launch a photo competition on this theme. Participants are invited to submit photographs that reflect their goal for the future.
Get some tips on taking great photographs here.
Prizes
• The winning entry will receive a top prize of €500.
• Four runners-up will each receive a prize of €250.
Entries will be judged by a panel including patients representatives and professional photographers. Winners will be announced in late January 2020.
EFNA plans to hold an exhibition of entries at the European Parliament in Brussels during Brain Awareness Week (March) [to be confirmed], and again at the European Academy of Neurology Congress in Paris (May).
The competition will be open until Wednesday, January 1st 2020 at midnight CET.
CLICK HERE FOR ENTRY FORM.
COMPETITION RULES
• Photos should reflect the #BrainLifeGoals theme .
• Photos must be submitted via the entry form here.
• Photos should be high-resolution (a minimum of 1MB and a maximum of 6MB file-size).
• Photos may be taken using a regular camera, smartphone or tablet.
• Entrants must provide their name, nationality and email address.
• Each entry must be entirely the original work of the contestant, must have a title, description and indicate the location in which the photo was taken.
• Entries submitted in a language other than English should include English translation.
• Entrants should be personally affected by a neurological disorder.
• Any person included in a photo must have given their express permission to be photographed.
• By submitting a photograph to EFNA the contestant agrees to grant EFNA, free of charge, the right to publish the photograph online and in other EFNA media.
• The contestant agrees to grant EFNA the right to publish the name, nationality and entry details provided with their entry.
• Closing deadline for entries is 1st January 2020 and all entries must be submitted electronically.
• The winning entries shall be announced in late January 2020
• Entrants under 16 years of age, must obtain your parent’s or guardian’s permission before entering the competition.
• A maximum of three entries may be submitted by each participant.
• The judges’ decision is final and no correspondence shall be entered into.
• EFNA reserves the right to disqualify any entry which breaches any of these rules.
• An independent judging panel shall select the winner and runners up.
• All information submitted will be stored in accordance with EFNA’s Data Protection Policy.
Image source: EFNA
Disclaimer: This article was written by a third party. It does not necessarily express the views of the Stroke Alliance for Europe. The party who issues this press release is entirely responsible for the accuracy of its information.
Nov 15, 2019
PRESS RELEASE ¦ FRIDAY, NOVEMBER 15, 2019 9:00 AM EST
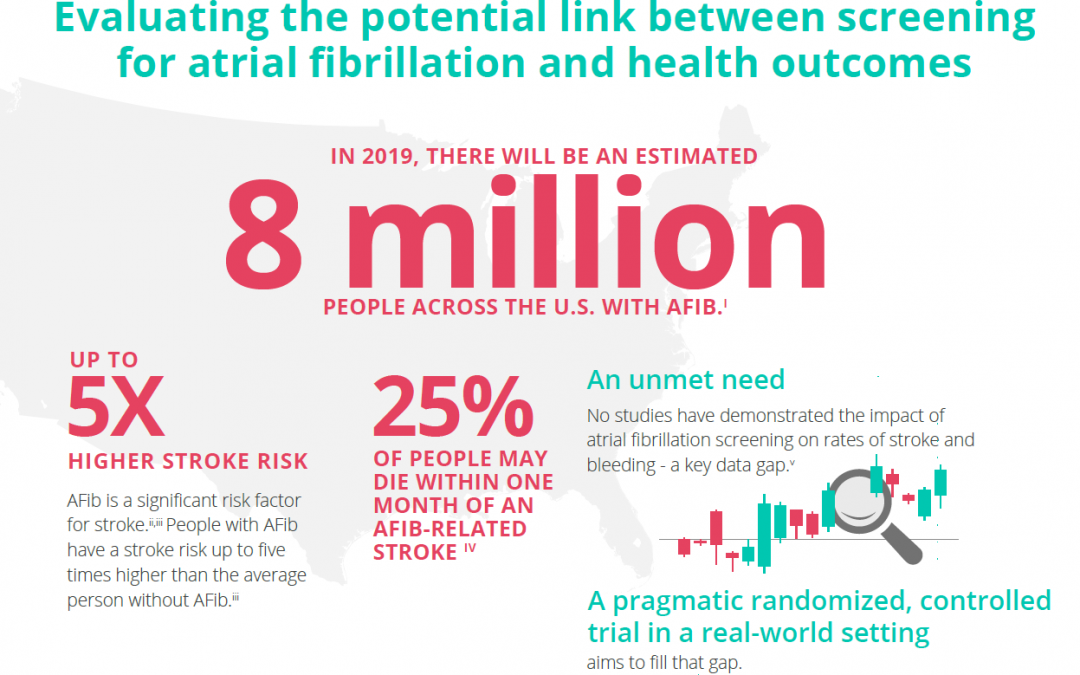
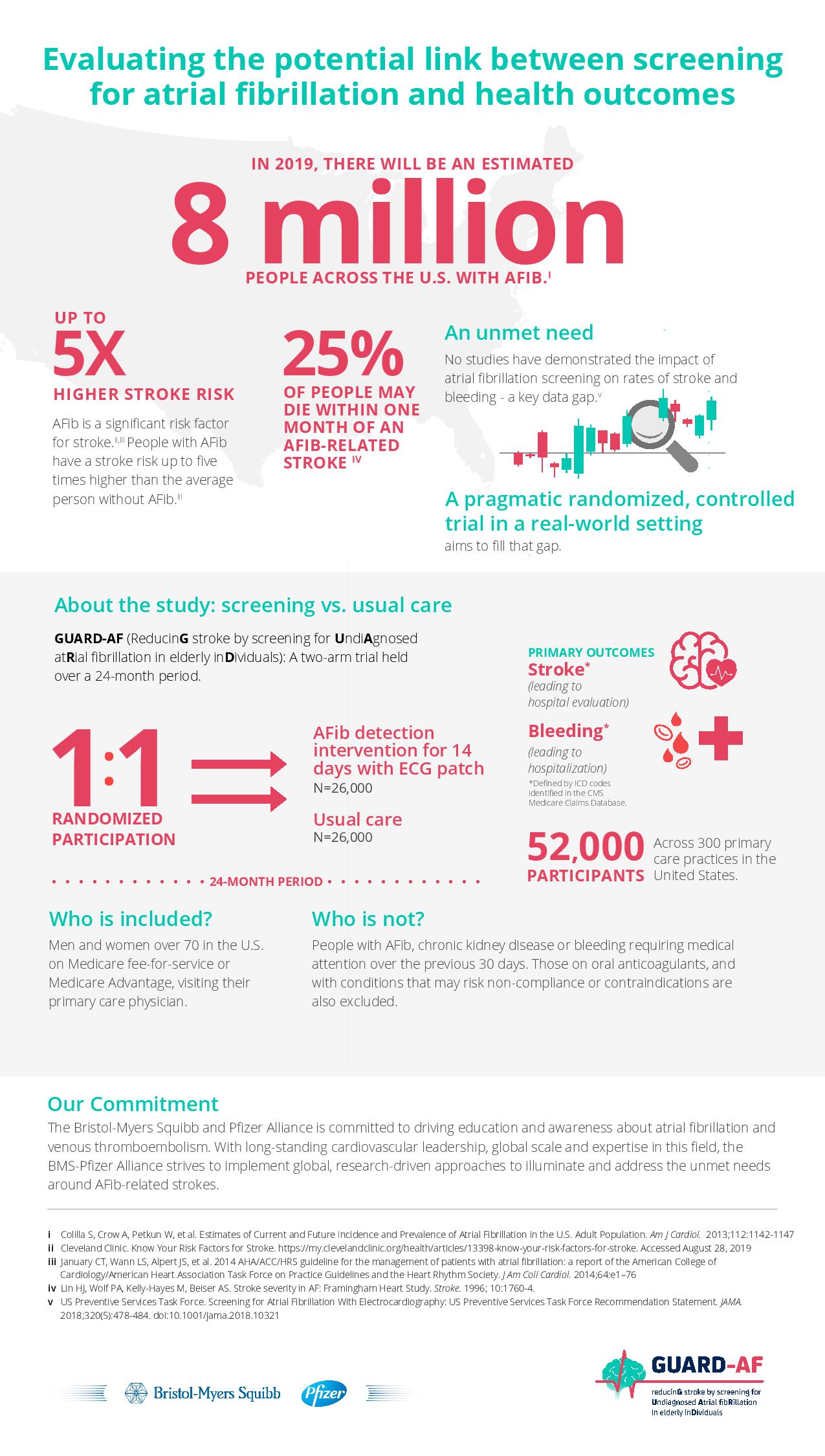
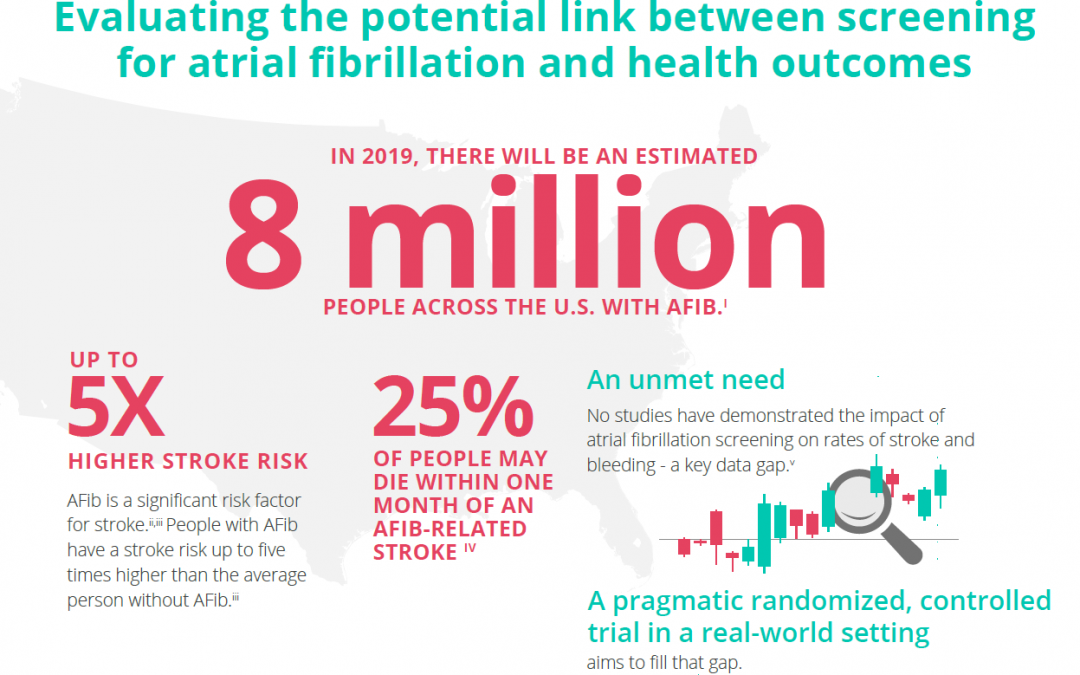
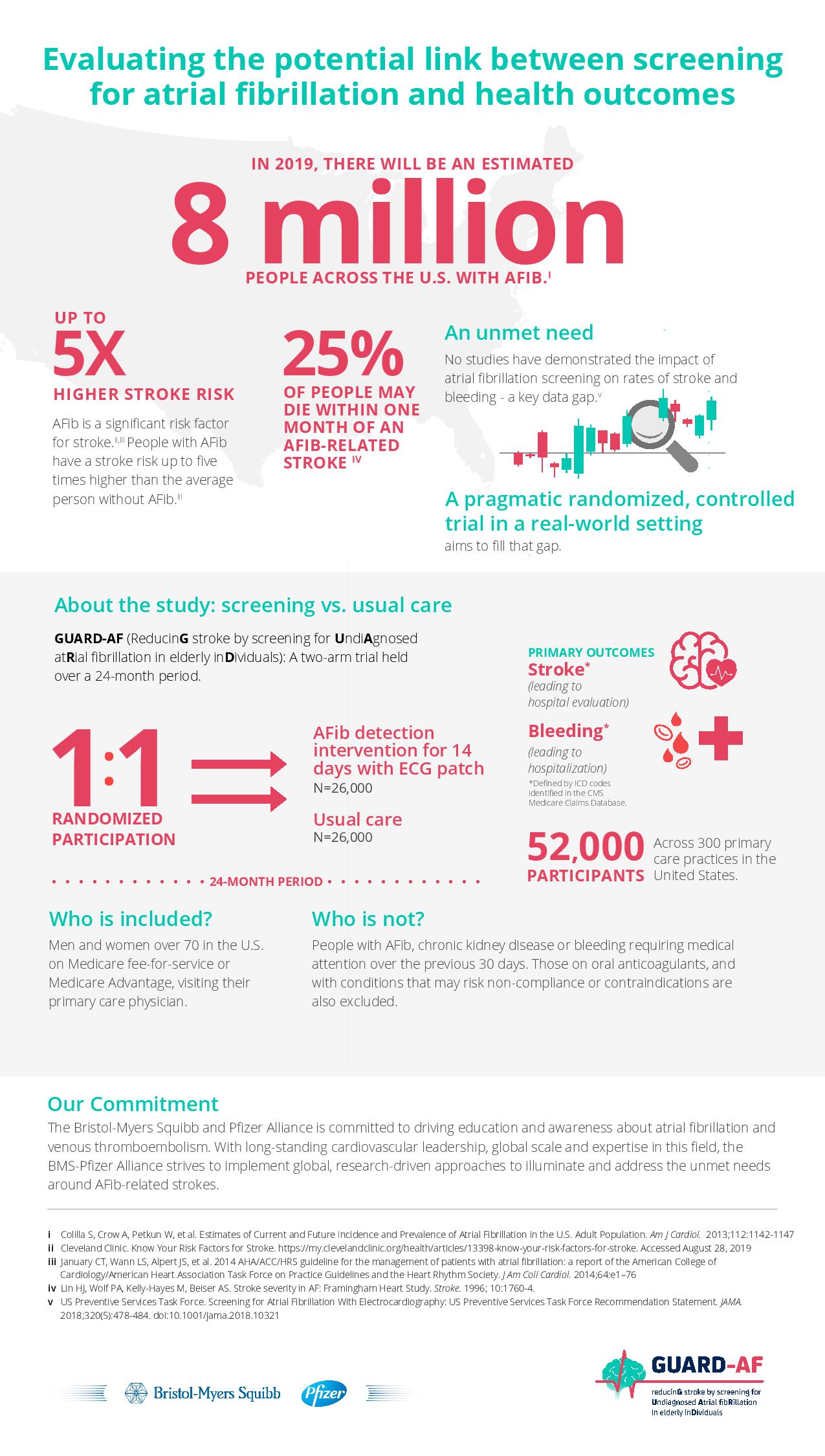
The Bristol-Myers Squibb-Pfizer Alliance today announced the initiation of a new randomized, controlled study, GUARD-AF (ReducinG stroke by screening for UndiAgnosed atRial fibrillation in elderly inDividuals). The study seeks to determine if earlier detection of atrial fibrillation (AFib) through screening in previously undiagnosed men and women at least 70 years of age in the U.S. ultimately impacts the rate of stroke, compared to usual standard medical care. This study will also assess potential bleeding leading to hospitalization, and therefore provide an evaluation of net clinical benefit or harm. AFib is the most common type of significant irregular heart rhythm, and it is estimated that 8 million people in the U.S. will be affected by AFib in 2019.i,ii AFib is a significant risk factor for stroke; stroke risk is up to five times higher in people with AFib than in those without it.iii,iv AFib can often go undetected, as it can be asymptomatic,i and some studies suggest that more than 25 percent of people who have an AFib-related stroke find out they have AFib after a stroke.v
“There is a real need for a study like GUARD-AF to assess the impact of screening for AFib on the crucially important outcome of stroke,” said Daniel Singer, M.D., Professor of Medicine at Harvard Medical School and Professor in the Department of Epidemiology at Harvard T.H. Chan School of Public Health, and an academic general internist at Massachusetts General Hospital. “This study has the potential to directly affect clinical practice and could lead to more AFib patients being identified and appropriately managed to avoid stroke.”
You can read the full press release here.
Disclaimer: This article was written by a third party. It does not necessarily express the views of the Stroke Alliance for Europe. The party who issues this press release is entirely responsible for the accuracy of its information.

Nov 14, 2019
Written by Alžbeta Husarovič, President of Porážka.sk
For this year’s World Stroke Day in Slovakia, a stroke support organisation Porážka.sk and a fashion stylist Andrej Kusalík organised a Charity Fashion Show. The event took place on 24th October 2019 in the Privee Lounge in Motešických Palace, in Bratislava, Slovakia.
 A successful Slovakian fashion designer Michael Kováčik created a T-shirt “Unbeaten” in three different outlooks for the Porážka.sk. These T-shirts were presented on a runway by Slovakian models and previous participants of the Miss Slovakia – Barbora Franeková, Magdaléna Šebestová, Eva Rezešová and Simona Brnová Slobodníková.
A successful Slovakian fashion designer Michael Kováčik created a T-shirt “Unbeaten” in three different outlooks for the Porážka.sk. These T-shirts were presented on a runway by Slovakian models and previous participants of the Miss Slovakia – Barbora Franeková, Magdaléna Šebestová, Eva Rezešová and Simona Brnová Slobodníková.
The main idea of the event was to auction money for the support of the Porážka.sk, with special focus on coveing treatment costs Peter Tatarko, an engineer who survived stroke in May 2018.
The main voice of the evening belonged one of TV moderators JOJ Lucia Wirthová. Apart from these designed T-shirts, the auction included a work of art by the academic painter Daniel Bidelnica and a painting by his wife Maria Bidelnicová as well. In addition to these two artworks also auctioned designer’s piece by Michael Kováčik, based on the auctioneer’s choice.
The evening was very successful and managed to auction around 6.500 EUR. The event was supported by leading bidders, celebrity photographer Petra Ficová, owner of Envy Lounge, Natalia Selveková and two anonymous auctioneers.
During the evening, the T-shirts were sold, bringing an additional sum of 800 EUR to Porážka.sk.
These beautifully designed T-shirts will continue to be sold on OZ Porážka.sk website www.porazka.sk, via Porazka.sk social media and on Zľavomat website, www.zlavomat.sk.

The funding that was generated through all of these activities will mainly be used for the treatment of Peter Tatarko, who overcame the defeat in May 2018. The treatment is expected to last for three intensive weeks. The cost of treatment is 3.500 EUR and Porážka.sk is very glad that it can help people through activities like this.
At the end, we would like to pass our massive thank you to everyone who participated and helped us raise the money. If you want to support our further work, please visit our website www.porazka.sk and purchase one of our beautiful T-shirts, knowing that you will not only get a very fashionable piece of clothing, but also help us continue with our very important work. Your purchase will be used for improvement of the lives of the stroke survivors in Slovakia.
A piece of the atmosphere at the event









Nov 14, 2019
Last month we were lucky enough to attend the Eye for Pharma Annual Patient Summit Europe in London. It was here that we also attended the first UK DrugStars patient organization event, where we proudly accepted a cheque for £500. This money was donated by UK patients using the DrugStars app.
DrugStars is an app, that helps you with your medicine. The app can help you remembering to take your medicine, but the truly special thing is that you also can donate money (FOR FREE) to patient organizations like us. So please download the app by this link https://drugstars.onelink.me/FN6p/83662720
#DrugStars #GivingByTaking #eyeforpharma #Patientsummit

Nov 6, 2019
SAFE’s Annual General Assembly will take place at the Sheraton Porto Hotel, R. do Ten. Valadim 146, 4100-476 Porto, Portugal, 29 November 2019. We would be delighted if members were able to attend.
The order of business will be as follows:
08.30-09.00 Registration
09.00-09.05 Opening welcome, Jon Barrick, President SAFE
09.05-10.00 Review of the year and forward view
10.00-11.00 General Assembly
11.00 Close
For further information, please see HERE in the Members’ Section and contact SAFE Secretariat at mail@safestroke.eu
Featured photo: SAFE General Assembly 2018, Berlin, Germany

Nov 6, 2019
Written by Amanda Jerelyn
Recovery after a stroke is very essential for a patient to make his coming back to life easy and simple for himself and his caretakers. Living a normal life after a stroke is hard to think about for many sufferers. People tend to get negative once they come back to their new life and do not accept the changes positively.
The story of Marina Krsmanovic from Serbia is very powerful in terms of reclaiming a life after stroke. Coming back to your life after recovery is a new beginning for you. It is completely achievable if you have a positive mindset. You can reclaim a normal life by following these expert approaches:
Returning to routine
It is barely impossible for some patients to accept the reality that their routine will not be the same anymore. Reclaiming life after stroke involves some drastic routine changes. Survivors should always believe in their goodwill in adopting major changes around them. Accepting your fate is the first step towards success in your new life. A patient who happily adapts to these routine changes will lead a life with fewer worries and more relaxation.
Positive perspective
Setting a positive approach towards everything that happens in your life is the key to happiness. Especially in your condition, positive thinking will only make you bloom. Once you accept your life as it is, things will get easier and better understandable by you. A positive mindset will also let you be your own motivator at times you’re alone.
Vernell Bradshaw is a stroke survivor. His motto is attitude is everything, and quite astonishingly, it is true. He lives his life with willingness and readiness. He also said that he never questioned why he had to go through it, but instead, he accepted it and gained enough strength to move on with his life enthusiastically.
Meditation is a great healer
After a stroke recovery, patients are highly advised by doctors to take care of themselves and make it a priority. Taking care of you means making sure all your needs and wants are being fulfilled. And your needs should firstly include taking out some time for meditation. Doing meditation routinely is an expert approach to live a life normally after a major stroke. Now medication may include doing light walk in the morning, doing yoga outdoors or indoors, or doing breathing exercises.
Physiotherapy benefit a lot
Individuals suffer from many symptoms like loss of memory, losing willpower, and losing the power of control that mainly includes limb control, after a stroke. Physiotherapy comes as very helpful in this particular case.
Physiotherapy mainly means a treatment for recovering patients that consist of physical techniques. It includes light exercises, massages, and treatments by heat to help with internal and external body movement with easiness.
So it is another expert approach to win back your life after stroke and start living it naturally.
Dressing method transformation
After a stroke, simple tasks such as dressing up or bathing become a hassle for survivors. Their frustration is genuine, but the expert approach would be to deal it with mindfulness and give it time.
Changing your way around things might help. For example, you can change clothes easily while sitting on a chair or bed instead of standing up. You can also choose to wear loose clothing so it can be less of a hassle. Putting your affected hand in the shirt’s sleeve first will give you more grips for wearing it properly.
Modify bathing equipment & tools
Now bathing is the second hardest task, but it can be made simpler by following some pro-tips. Always remember that baths are harder to take after a stroke, so you should opt for showers. Replace your usual bathmats with suction-cupped bathmats to avoid slipping. Always keep someone or a bell in your reach to have instant help when in an emergency.
Avoid driving at maximum
Driving after a stroke can’t be easy or normal. In some extreme cases, it is not advised for some patients after recovery by their physiotherapists and doctors. But if you must, then firstly you need to have the authorities informed and have a test ride with them for surety. Then you need to modify your car according to your hand, which is not paralyzed. Safety tip is to have someone ride along with you at all times to ensure you don’t accidentally meet some severe strokes.
Attending group sessions
People after recovery from a stroke become bitter and angry because of isolation and because they can’t do things they used to do before by themselves. It is entirely understandable, and an expert approach would be to attend sittings. Sessions related to life after stroke will brighten-up your spirit. Because you will now feel linked to many others and feel relaxed knowing you’re not suffering alone in this situation. Attending group sessions will rise-up your morale and motivate you towards all the positive things in life to cherish.
Keep challenging yourself
A patient who survives a stroke and comes home after recovery needs the most challenges in their life to keep moving forward. Think of it as you always come first in all the racing marathons and suddenly racing marathons stopped happening, how would you feel? You’ll feel stuck in between. So daily challenges, no matter big or small, keeps your life going on a steady path. So survivors should always keep looking for problems and try their best to overcome them effectively.
These were some useful approaches that you can consider after recovering from a stroke. And life is undoubtedly reclaimable after a stroke. You just have to be willing to live it fully. Living a normal life is not a dream, but it’s a mission for survivors, and you’ll get through with it too.
Author bio:
 Amanda Jerelyn is currently working as a health & wellness tutor at King Essay.
Amanda Jerelyn is currently working as a health & wellness tutor at King Essay.
Her professional writing services include nursing dissertation through which she gained much popularity in her field and she occasionally contributes content to Guide2Write. Amanda writes with full contribution and enthusiasm, which makes her stand out from the rest.
Nov 1, 2019

Austin Willett, Chief Executive Officer, Different Strokes
“Stroke is still thought of us something that only happens to elderly people. Yet more than 25% of strokes happen to people who are of working age and younger, and in the specific 35-54 age range, strokes are increasing by approximately 2% per year. Despite this, when stroke is portrayed in the media it is almost always in the context of an older person suffering a stroke, and this further entrenches the view that it is something that is not experienced by younger people. At Different Strokes we have helped to tackle this misconception, and a recent Stroke Association television advert also featured a number of young stroke survivors. ” said Austin Willett, Chief Executive Officer at Different Strokes, a stroke support organisation from the UK.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
AW: Clearly though there is still a very long way to go, demonstrated by the results of a survey which we commissioned this year. In this survey, 84% of people thought that only 1 in 50 strokes happened to people under the age of 65, while it is actually more than 1 in 4.
The marginalisation of stroke survivors is an ongoing problem. Stroke is especially isolating for working age people; often with young families to support and relying on employment but suddenly unable to work. Ensuring that there is much greater recognition of younger stroke is, for us and the people we support, the most important issue.
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
AW: There are no easy answers to this, and because stroke affects everyone differently there is not a solution that will work for all stroke survivors. But broadly speaking, we would like to see:
- Much greater understanding of the prevalence of stroke in younger people. Where there is ignorance about this issue, this can lead to misdiagnosis. Too often is a stroke among this age group classified as a ‘brain bleed’ or something other than stroke. This can lead to people waiting for extended periods of time before receiving appropriate stroke rehabilitation, or not receiving any at all.
- Rehabilitation which focuses more on the specific needs of younger stroke survivors. Younger stroke survivors must learn to accept newfound physical, emotional and cognitive limitations, as well as changes to virtually every aspect of life – wellbeing, perceived quality of life, communication, mobility, employment, independence, social life and relationships. Rehabilitation needs to reflect this, and not merely be focused on the basic functions of self-care which permit a stroke survivor to return home.
- Recognition that ongoing recovery of stroke is a long-term, and sometimes lifetime, process. Too often we have heard stroke survivors being told that they have plateaued to explain why their post-stroke rehabilitation has been discontinued, and a further myth about stroke is that after 6 months post-stroke ongoing recovery will cease. But post-stroke recovery trajectories vary and shift over time, and at Different Strokes we see stroke survivors of working age return to work and rediscover skills and interests which buck their disabilities long after their stroke.
SAFE: Please tell us more about your organisation.
AW: Different Strokes is a registered charity which supports younger stroke survivors and their families, primarily of working age (18-65). This group has historically been overlooked, receiving limited rehabilitation and struggling to find the emotional support combined with the practical help required to help reclaim their lives. Different Strokes was founded in 1996 to address this, and over the last 23 years has made huge steps in raising awareness of young stroke.
Amongst the services we provide are a network of peer support and exercise groups, an online support group, a telephone information line, printed materials, and age appropriate resources for children whose Mum or Dad has had a stroke.
We also seek to raise awareness of issues that specifically effect younger stroke survivors and will work collaboratively with third parties where it is in our mutual interests to do so.
The ethos of Different Strokes is one of ‘survivors supporting survivors’, with peer support running through all that we do. Half of our staff and trustees are stroke survivors, as are the vast majority of volunteers who run local groups and support us in other ways.
We receive no funds from central or local government, so have to raise all our funds from individual donations, fundraising events, legacies, grants from trusts and foundations, corporate support, and self-generated income such as through our online shop.
*Image source: https://differentstrokes.co.uk/stroke-information/information-pack/

Oct 29, 2019
Today is the World Stroke Day and the global campaign’s slogan is „1 in 4 of us will have a stroke. #DontBeTheOne“.
SAFE supports the global campaign, as we do every year. At the same time, we recognise and acknowledge the struggle of those among us who were unlucky enough to become #theOne from the World Stroke Day slogan.
We represent the voice of stroke survivors and their families through Europe.
Believing that all these voices must be heard, SAFE organised a series of interviews with the stroke support organisation representatives from around 30 European countries. Today we are able to present you with their unique insight into life after stroke issues, country by country.
We hope you would help us spread the news and share these country insights. Click HERE to open and download the compilation of interviews with key people from European stroke support organisations.









 A successful Slovakian fashion designer Michael Kováčik created a T-shirt “Unbeaten” in three different outlooks for the Porážka.sk. These T-shirts were presented on a runway by Slovakian models and previous participants of the Miss Slovakia – Barbora Franeková, Magdaléna Šebestová, Eva Rezešová and Simona Brnová Slobodníková.
A successful Slovakian fashion designer Michael Kováčik created a T-shirt “Unbeaten” in three different outlooks for the Porážka.sk. These T-shirts were presented on a runway by Slovakian models and previous participants of the Miss Slovakia – Barbora Franeková, Magdaléna Šebestová, Eva Rezešová and Simona Brnová Slobodníková.












 Amanda Jerelyn is currently working as a health & wellness tutor at King Essay.
Amanda Jerelyn is currently working as a health & wellness tutor at King Essay.