Oct 26, 2019
Fundació Ictus and the four associations who represent the several local patient groups from Catalonia met last Saturday, 26th October to celebrate the World Stroke Day all together. It was the first time Fundació Ictus and the four associations celebrated together that day in Lleida, one of the four major cities of the country.

Xavier Trias, Fundació Ictus’ president, in the middle of the image, surrounded by the four associations who represent patients in Catalonia
All of them read an ensemble manifesto to speak out all people’s necessities related to this disease. In Catalonia, stroke is the first cause of mortality among women and the second one in men. Moreover, stroke is the principal cause of disability, so it becomes a health and social problem for people who suffered one and their families.

People from the four Catalan patient associations read an ensemble manifesto
Xavier Trias, Fundació Ictus’ president, pointed out the importance of collaboration of all the Catalan association that they should work together in order to be stronger. Furthermore, Trias remembered the relevance of prevention to be successful in avoiding the disease and the importance of rehabilitation to minimize long term damages. In the same meeting, there were politicians who listened very carefully to all the demands expressed.
This event came after another one, which took place last Wednesday 23th October in Barcelona. One of the most important concert halls, Luz de Gas, held a live music concert in support of stroke survivors.
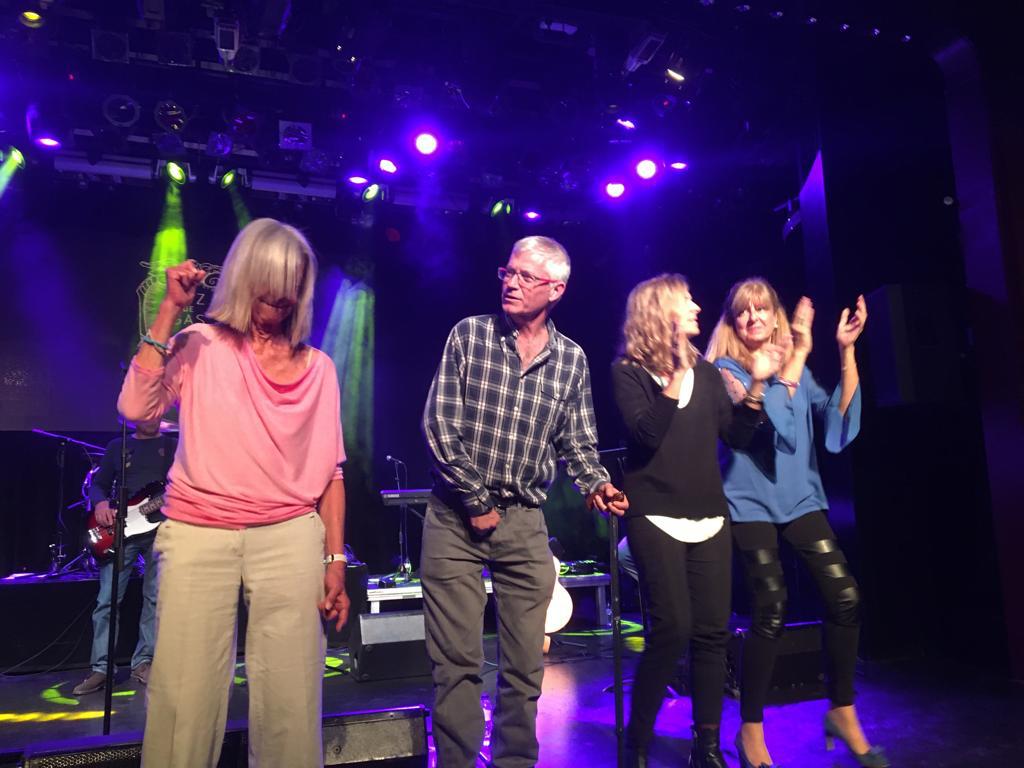
The concert hall Luz de Gas, where the live music concert was held in support of stroke survivors
Oct 25, 2019
Oruen, CNS medical publication and audio-visual platform, would like to recommend to your attention the latest round table discussion about learnings from the ESUS trials – Jesse Dawson, Martin Grond & Maurizio Paciaroni.
Faculty:
Jesse Dawson MD, Professor, Institute of Cardiovascular & Medical Sciences University of Glasgow, Scotland
Martin Grond MD, Professor, Department of Neurology Kreisklinikum Siegen, Teaching Hospital of the University of Marburg, Germany
Maurizio Paciaroni MD, Neurologist, Stroke Unit and Division of Cardiovascular Medicine, Santa Maria della Misericordia Hospital, University of Perugia, Italy
This video discusses the role of NOACs for secondary prevention of stroke in the setting of embolic stroke of unknown source
Following completion of this activity, learners will be able to:
- Outline key features and results of the ESUS trials, with focus on NAVIGATE ESUS and RE-SPECT ESUS
- Recognize differences in study outcomes
- Summarise implications of ESUS as a concept for use in clinical practice

Oct 25, 2019
 “Stroke survivors in the UK are going without vital care and support. There are 1.2 million stroke survivors across the UK, but sadly 45% of people feel abandoned after leaving hospital” says Juliet Bouverie, Chief Executive of the Stroke Association UK.
“Stroke survivors in the UK are going without vital care and support. There are 1.2 million stroke survivors across the UK, but sadly 45% of people feel abandoned after leaving hospital” says Juliet Bouverie, Chief Executive of the Stroke Association UK.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
JB: We need to put the spotlight on long-term stroke care and rehabilitation. As anyone dedicated to helping stroke survivors rebuild their lives will recognise, the condition is extremely complex. People affected by stroke need rehabilitation that covers emotional support, help with finances, support services for carers, as well as physiotherapy, and speech and language therapy. Sadly, a recent Stroke Association survey of stroke survivors across the UK found that, in the aftermath of their stroke, only 18% of stroke survivors were confident that they would get enough support to make a good recovery. And 80% of stroke survivors told us they initially feared they would be sent to a care home.
Stroke causes a wide range of physical, communication, emotional and cognitive difficulties, and more than half of survivors report fatigue, memory and concentration difficulties, anxiety or low mood. Time and again we’ve seen thousands of people adapt to a new life after stroke. But it’s only possible with the right specialist support – and a ton of courage and determination. But the sad truth is that thousands of stroke survivors do not receive the support they need with their recovery when they leave hospital. There are huge regional variations in stroke support and care, which leaves stroke survivors at the mercy of a postcode lottery. On average, stroke survivors receive less than half the amount of rehabilitation recommended by national guidelines and many report feeling ‘abandoned’ after leaving hospital.
We know there are hospitals, stroke units and dedicated professionals leading the way for stroke care and support right across the UK. But too many stroke survivors are being let down because they aren’t given ongoing support to rebuild their lives. We want everyone affected by stroke to have the rehabilitation and long-term support they need, no matter where they live. No stroke survivor should be denied the chance to rebuild their life.
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
JB: We know that the number of strokes is set to increase, and that too many stroke survivors aren’t getting access to the services they need to make their best possible recovery after they leave hospital. At the moment, we know there’s too much variation in the quality and coverage of care: too many of therapies recommended by clinical guidelines aren’t available across the country.
Stroke is also a hugely expensive condition, costing around £26bn a year across the UK. If we don’t act to roll out some of the actions we know can stop stroke before it strikes, save lives and prevent serious disability, the costs will spiral. We can’t afford not to act.
We want everyone affected by stroke to have access to the support they need and should expect, in line with national guidelines. That’s why we’re working across England, Scotland, Wales and Northern Ireland to support and drive changes which will improve the lives of people affected by stroke. In England, for example, we’re working closely with NHS England to deliver the Long Term Plan for the NHS, which includes the National Stroke Programme.
This Programme supports health and care services to make improvements from prevention and treatment right through to rehabilitation and long-term support after leaving hospital, including psychological support for stroke survivors. Our focus now is to ensure promised improvements are delivered.
SAFE: Please tell us more about your organisation.
JB: We’re here to support people to rebuild their lives after stroke. We believe everyone deserves to live the best life they can after stroke. We want to drive better outcomes in stroke prevention, treatment and lifelong support for everyone affected by stroke
We provide specialist support, fund critical research and campaign to make sure people affected by stroke get the very best care and support to rebuild their lives. The Stroke Association also offers vital support and information through our Stroke Helpline. My Stroke Guide is our online community of over 11,000 people affected by stroke, which many people said helps with their recovery.
Rebuilding lives after stroke is a team effort. It takes the determination of stroke survivors and carers, the generosity of supporters and the dedication of the healthcare and research communities to get there. We work hard to connect everyone in the stroke community so that people can live the best life possible after stroke. We have a number of stroke clubs and groups which provide essential long-term peer support to stroke survivors, carers, family and friends.
The Stroke Association’s campaign, Rebuilding Lives, aims to change perceptions about stroke, and reach more people who need support with their recovery. We hope the campaign, which includes TV advertising, will help us get our message out to people who need help and support, and raise awareness that it’s possible to rebuild lives after a stroke. To find out more, visit https://www.stroke.org.uk/rebuilding-lives

Oct 20, 2019
Author: Anna Tsiakiri, PhD, Psychologist from the Greek stroke support organisation, Hellenic Alliance for Stroke
This weekend, the Hellenic Alliance for Stroke in cooperation with the Hellenic Neurological Society, Postgraduate Program “Stroke” of Democritus University of Thrace, Hellenic Society of Cerebrovascular Diseases, Department of Educational and Social Policy of Macedonia University co-organized a two-day scientific event on 19th & 20th October 2019.

The scientific part of the event consisted of lectures from distinguished speakers specialised in Stroke, both in terms of medical care and rehabilitation.
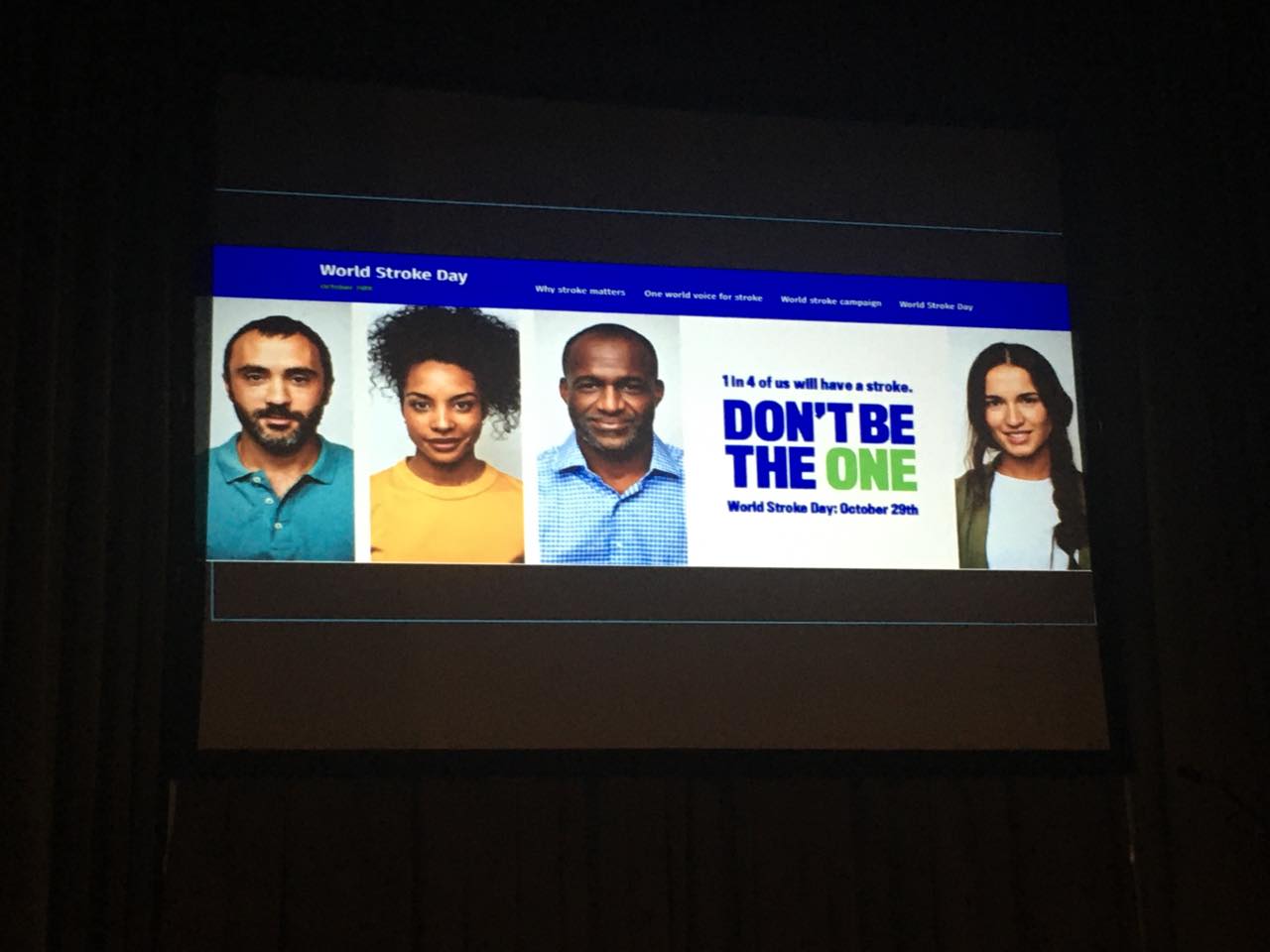
The informative event, that was addressed to general public, aimed to provide useful information about preventing Stroke- how to recognize stroke symptoms, how we should react. A special tribute was made to stroke survivors.
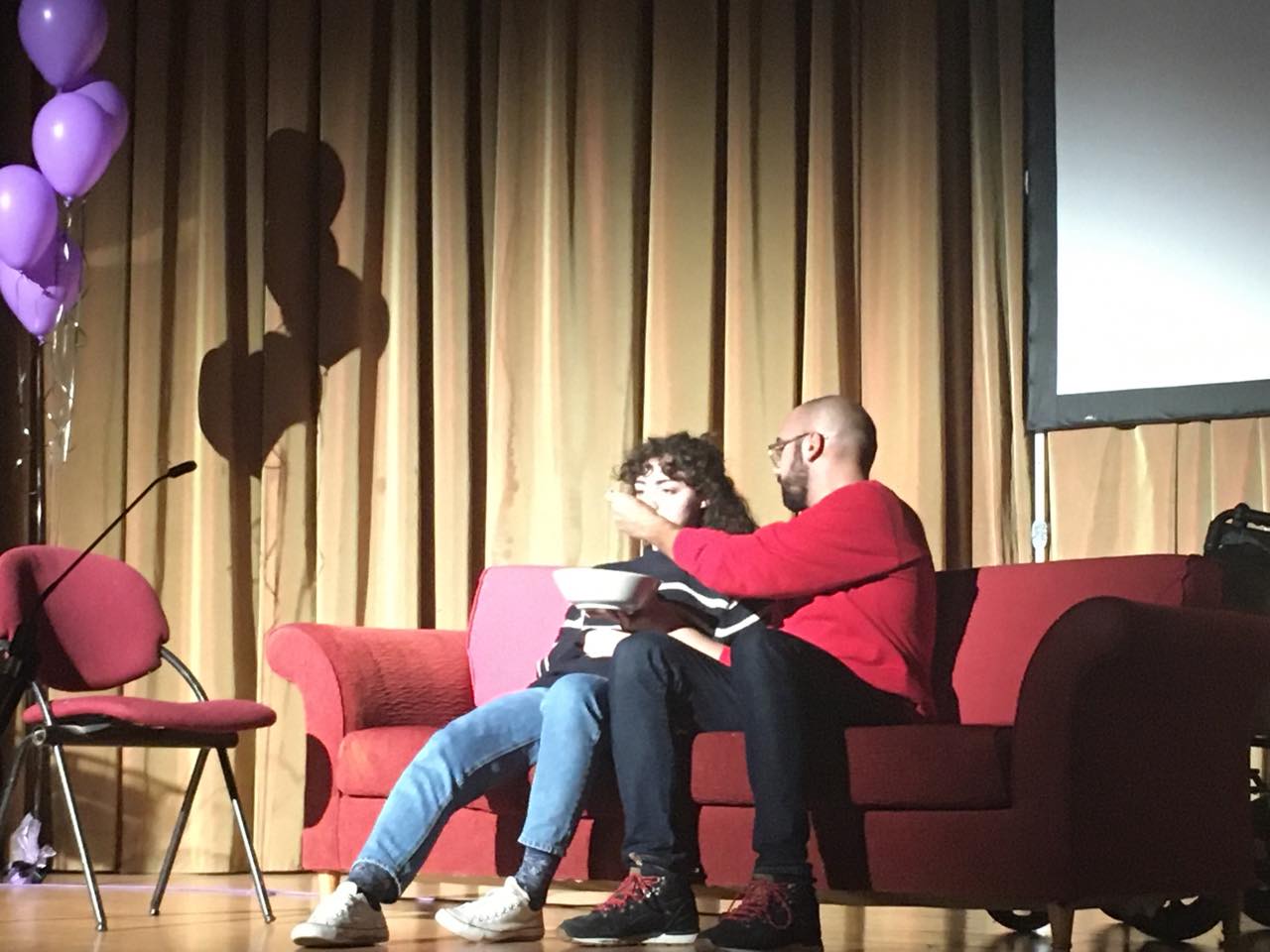
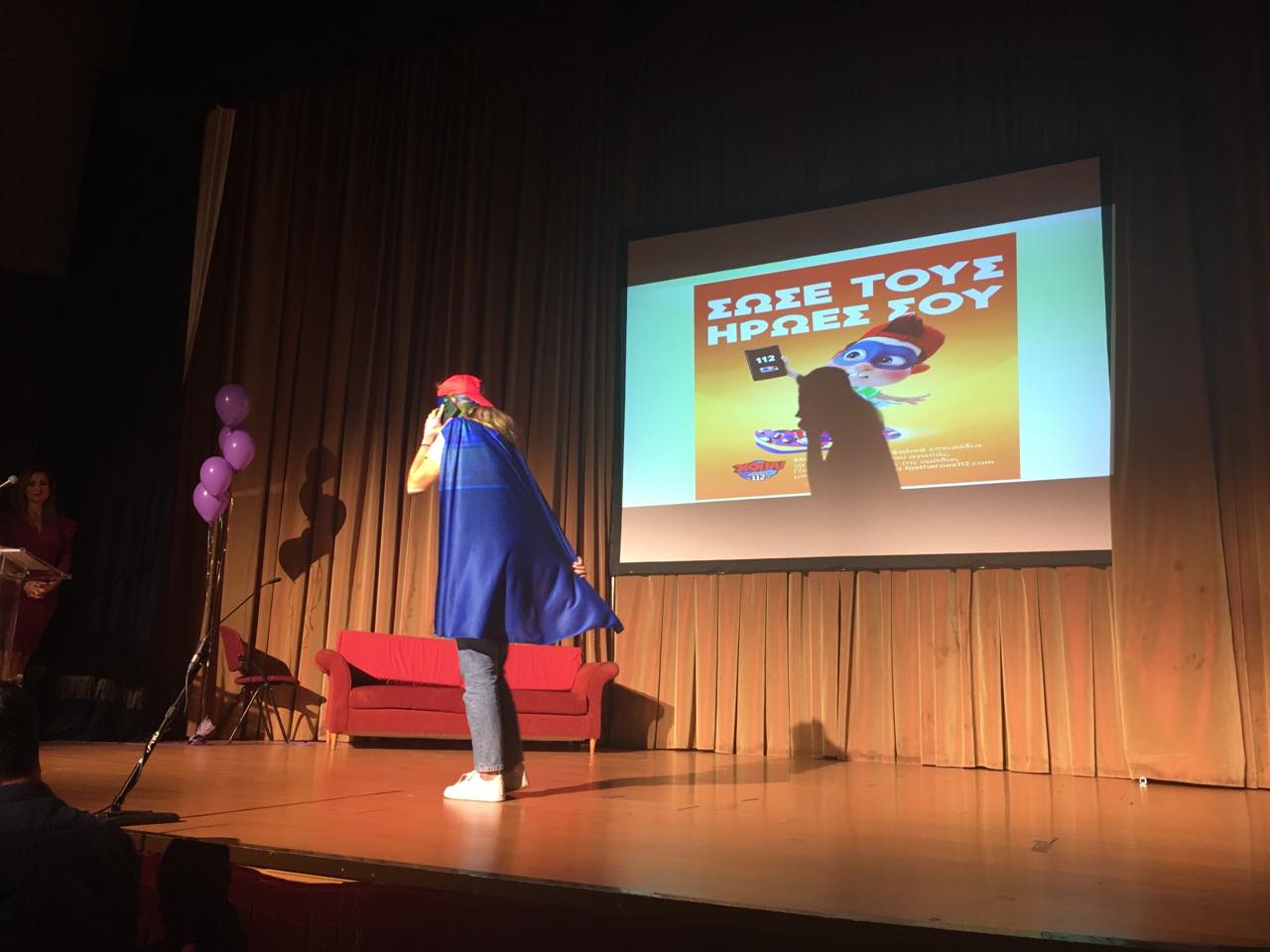
The theatrical group of students of Democritus University has prepared a performance in order to raise awareness of stroke prevention, while HOPA/FAST heroes presented their great work in different parts of Greece.


Hellenic Alliance for Stroke presented their activities and the role of SAFE.
Finally, the event was closed with a Latin performance.


Oct 18, 2019

Chris Macey, Head of Advocacy for the Irish Heart Foundation
“The rate of death and permanent severe disability from stroke in Ireland has been reduced by more than 20% in the last decade. But hundreds of people are still dying every year when their lives could be saved. And thousands more are not receiving basic services that would enable them to make the most of life after stroke” says Chris Macey, Head of Advocacy for the Irish Heart Foundation and a SAFE Treasurer.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
CM: Irish stroke services compare well internationally in the vital early period after stroke occurs. But as soon as a person’s life is saved they typically start to regress through poor access to basic therapies in hospital. In therapy terms, patients then effectively walk off a cliff after they pass through the hospital gates – for most physiotherapy, speech and language or psychological services are grossly inadequate or non-existent unless they can afford to pay themselves.
As a result, more people than ever before are surviving stroke only for many to have their recoveries squandered by the failure to deliver the therapy services either in hospital or the community that will help rebuild their lives.
These services require upfront investment, but we do not need to spend more money on stroke. We just have to spend what we have in a different way. For example, our research showed that out of a direct cost of stroke to the Irish State of €557 million a year, up to €414 million was spent on nursing home care and less than €7 million on the community rehabilitation that can keep people in their own homes.
In other words the system starves vital acute and rehabilitation services of funding only then to spend huge amounts of money after the time patients can be helped most.
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
CM: We need to recalibrate expenditure on stroke services in Ireland, through upfront investment in acute services and a much greater priority for community rehabilitation services.
The average onset of stroke here is at age 73 and because we will have 50% more 73-year-olds here within the next decade it is vital that we futureproof acute services, first by improving the standard of our stroke units – just one out of 28 fully meets ESO guidelines at present. We need around 200 extra therapists to meet current needs. We also need to invest in thrombectomy services that Irish doctors helped pioneer and to expand Early Supported Discharge (ESD) services that get patients home quicker and improve outcomes.
The development of ESD will also start to address the chronic deficits in terms of therapists working in the community where there are few champions at present for better services. In addition, we have helped to spearhead the development of community rehabilitation teams – working across neurological conditions – to continue therapies after ESD treatment has been completed. Their development in pilot locations and then nationally has to be speeded up however to address the huge unmet need among stroke survivors in the community.
More resources must also be provided to support stroke survivors living at home – the vast majority of stroke support in our country is provided by the Irish Heart Foundation without State assistance outside Dublin and the north west of the country.
SAFE: Please tell us more about your organisation.
CM: The Irish Heart Foundation is Ireland’s national charity fighting heart disease and stroke. Our main activities include:
• Provides information on heart health to the public and media
• Supports patients in managing heart disease and stroke
• Provides heart health programmes in schools and workplaces
• Co-ordinates the training of medics and the public in emergency lifesaving skills (CPR)
• Supports research, education and development in the medical profession
• Advocates for better patient treatment and services and for public health measures that protect and enhance cardiovascular health
We have been particularly effective in developing progressive public health policy in Ireland. We secured improvements to stroke services that have reduced mortality by 20% and permanent severe disability by more than a quarter in the last ten years.
We were a leader of the coalition that ensured Ireland became the first country in the world to ban smoking in the workplace that has saved a life a day in Ireland for 15 years since and that has reduced the youth smoking rate from 41% to 12%.
We also secured Ireland’s sugar sweetened drinks tax, along with restrictions on junk food marketing to children on TV and radio. In addition, we ensured that defibrillators are present on all flights into and out of Ireland and we helped secure major changes to the law to reduce the harm done by alcohol.





 “Stroke survivors in the UK are going without vital care and support. There are 1.2 million stroke survivors across the UK, but sadly 45% of people feel abandoned after leaving hospital” says Juliet Bouverie, Chief Executive of the Stroke Association UK.
“Stroke survivors in the UK are going without vital care and support. There are 1.2 million stroke survivors across the UK, but sadly 45% of people feel abandoned after leaving hospital” says Juliet Bouverie, Chief Executive of the Stroke Association UK.