Mar 12, 2019
First published on ScienceDaily.com
Tumult in the bacterial community that occupies your gut — known as your microbiome — doesn’t just cause indigestion. For people recovering from a stroke, it may influence how they get better.
A recent study by Allison Brichacek and Candice Brown, researchers in the West Virginia University School of Medicine, suggests that stroke patients’ microbiomes — and even the structure of their guts — may still be out of kilter a month after the stroke has passed.
“We’re interested in the gut-brain axis — how the gut influences the brain and vice versa,” said Brichacek, a doctoral student in the immunology and microbial pathogenesis graduate program. She presented her findings at the International Stroke Conference in February.
Previous studies indicated the immediate effects a stroke can have on someone’s microbiome, but they didn’t explore whether these effects lingered. To find out, Brichacek, Brown and their colleagues — including Sophia Kenney, an undergraduate majoring in immunology and medical microbiology, and Stan Benkovic, a researcher in Brown’s lab — induced a stroke in animal models. Other models — the control group — didn’t have a stroke. The researchers compared the two groups’ microbiomes three days, 14 days and 28 days post-stroke. They also scrutinized their intestines for microscopic disparities.
Bacterial friend or foe?
One of the researchers’ discoveries was that a certain family of bacteria — Bifidobacteriaceae — was less prominent in post-stroke models than in healthy ones both 14 and 28 days out. If the name of the family sounds familiar, that’s probably because Bifidobacterium — a genus within the Bifidobacteriaceae family — is a common ingredient in yogurt and probiotics. These bacteria are known for supporting digestive health and may be associated with better outcomes in stroke patients.
Read the full article here.

Mar 11, 2019
Sharing #LifeGoals has become a popular trend on social media. A campaign from the European Federation of Neurological Associations [EFNA] and supported by many organisations across Europe will put a new spin on the trend by instead seeing patient advocates and supporters share their #BrainLifeGoals.
The #BrainLifeGoals campaign will raise awareness of the impact of neurological diseases by exploring the dreams and aspirations of those living with a brain disorder.
You can find out more about the campaign at www.efna.net/brainlifegoals and by following the #BrainLifeGoals hashtag on social media.

Mar 7, 2019
The German Stroke foundation started its work in January 1993. To celebrate the anniversary the foundation launched a new campaign: “I set a sign.” A newly designed website went online in October and the Integrated Care Project “STROKE OWL” enrolled the first patients.
Author: Ina Armbruster
 “I set a sign.”
“I set a sign.”
A red stripe above the eyebrow represents the stroke. A sign that celebrities, stroke victims and supporters set to raise awareness and show their solidarity towards stroke-victims. The campaign “I set a sign” was launched in May 2018 at the “Rosenball”, a significant charity event for the German Stroke Foundation in Berlin. During this event many guests had their picture taken with a red stripe above their eyebrow and uploaded their “sign” on social media or the campaign-page www.schlaganfall.de.
The campaign was running on many different channels. The local billboard company supported the foundation by offering rent-free billboards for a couple of weeks which were set up all over Gütersloh, the hometown of the foundation. Thanks to the cooperation with the TV channels of the RTL Group more than 100 million viewers have seen the TV-spot “I set a sign” so far. The advertisement has been published in many magazines with an edition of 1,5 million in total. People who have set a sign were portrayed with their individual stories on facebook once a week. Up to a couple of hundred users liked or commented on these posts.
The foundation used the campaign to raise awareness of stroke – because everyone can have a stroke, regardless of age, gender or social background.
New website
 The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters.
The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters.
Additionally, the website is now accessible for mobile devices as well. In 2019 the website will be updated with more information. The foundation also plans to add further technical features. www.schlaganfall-hilfe.de
Project “STROKE OWL”
 The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke.
The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke.
About the project:
- A specialised stroke case manager gets in touch with the patient at the stroke unit. The patient can take part in the program if he or she fulfils certain enrolement criteria. The case manager visits the patient during rehab and at home.
- All case managers have experience with stroke patients. Most of them are nurses or therapists with further education in case management.
- The case manager informs patients and their families about everything they need to know after having a stroke and gives them advise and support. The manager organises the treatment, helps filling out applications, and looks after the patient in general.
- The manager supports the patient for one year. The foundation´s goal is to enrol 2000 patients in the program.
By proving the advantages of a case management not only for the patients but also for the health care system in general the German Stroke foundation wants to support the establishment of stroke case management, which in the end is payed by the insurance companies.
Looking forward to 2019
 The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning:
The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning:
– seminar for parents of children who had a stroke
– implementing a second case manager in Germany for children who had a stroke and their families
– continuing the project “STROKE OWL”
– raising attention to the topic with a campaign for the “Day against stroke” in May (with a focus on “The invisible consequences of stroke”, e.g. concentration-problems, emotional imbalance or neglect)
– 4-day workshop for young stroke patients between 18 and 50
and much more…

Feb 27, 2019
This news first appeared in the WSO Newsletter
The World Stroke Organization is proud to share its most recent and much expected publication: the Global Stroke Fact Sheet.
The 10-page document overviews the best available scientific evidence to provide reliable and up to date data on stroke and its impact around the world. Using reliable and consistent stroke data to support stroke advocacy helps to build awareness of the scale of the disease and supports the call for urgent action at global, regional and national levels.
The values in the document have all been extracted from the most current Global Burden of Disease Stroke Statistics Worldwide for the year 2016. The present document and all its subsequent revisions are reviewed and approved by the WSO leadership.
We hope that Global Stroke Fact Sheet will be a valuable resource and a useful point of reference in your work, practice, and research.
We invite you to share the document with your colleagues, students and partners. Thank you for your continuous support for the work of WSO.
You can access and download the Global Stroke Fact Sheet here
For more information please visit WSO website.

Feb 20, 2019

The Stroke Alliance for Europe (SAFE) invites you to attend the event ‘Joining forces to prevent and control non-communicable diseases: The role of policy in tackling stroke’, under the patronage of the Romanian Presidency of the Council of the European Union (#RO2019EU), which will take place on 28 March 2019, in Brussels, at the European Committee of the Regions. The event will be organised by SAFE in collaboration with the European Stroke Organisation and the Romanian National Stroke Association.
The event will look into the role of policy and policy stakeholders in combating stroke-related challenges and addressing the burden of stroke, as well as in achieving the ambitious targets of the ‘Stroke Action Plan for Europe 2018-2030’. The discussions will be integrated into the expected health priorities for the Romanian and upcoming Finnish and Croatian presidencies as well as current and future EU action for preventing and controlling non-communicable diseases.
The Action Plan focuses on seven key domains, namely primary prevention, organisation of stroke services, management of acute stroke, secondary prevention, rehabilitation, evaluation of quality and outcomes as well as life after stroke. It outlines four overarching targets to be achieved by all European countries and health systems by 2030, which are complemented by further specific targets set for each of the seven domains. SAFE and ESO are currently pursuing its dissemination and implementation at national, regional and local levels.
With an expected 35% increase in the incidence of stroke in Europe by 2035, as highlighted in the Burden of Stroke in Europe Report, this conference represents an important opportunity to bring together European, national and local policy-makers and other key stakeholders to address the disparities across the stroke care pathway between and within European countries.
REGISTRATIONS
Registrations for our event are now open! If you are interested in joining us on 28 March at the CoR please register here. On the other hand, if you cannot come to Brussels but would like to follow the live streaming of the event, you can show your interest here.
PROGRAMME
The event programme will be published soon.
THE SPEAKERS

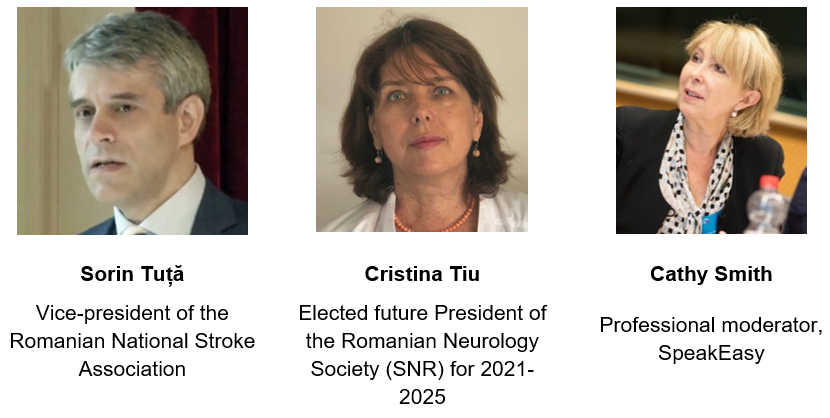
To view more information on the speakers click here.
ORGANISERS
The event will be organised by SAFE in collaboration with the European Stroke Organisation (ESO) and the Romanian National Stroke Association (ANRS).

About SAFE
SAFE is an umbrella organisation that represents a range of stroke patient organisations across Europe that were affected by stroke. SAFE’s vision is to work towards reducing the number of strokes in Europe as well as ensuring that everyone who is affected by stroke gets the help and support they need.
By combining the resources of patient organisations across Europe SAFE is working for better stroke prevention, more effective stroke care, greater public awareness and increased research activity within Europe.
About ESO
ESO is a pan-European society of stroke researchers and physicians, national and regional stroke societies and lay organisations. The aim of the ESO is to reduce burden of stroke by changing the way that stroke is viewed and treated. ESO serves as the voice of stroke in Europe, harmonising stroke management across the whole of Europe and taking action to reduce the burden of stroke regionally and globally.
About ANRS
ANRS is an independent, not-for-profit, non-governmental and apolitical Romanian association of physicians with scientific, medical and social goals regarding stroke prevention and management optimisation in accordance with the European and WHO standards. The association organises congresses, conferences, round tables, practical demonstrations and symposia that seek to promote up-to-date stroke education, according to the latest scientific research and validated therapeutic progress.
ENDORSEMENTS
The event will be held under the patronage of the Romanian Presidency of the Council of the European Union and hosted at the European Committee of the Regions (CoR).

About the Romanian Presidency of the Council of the European Union
Romania will hold the Presidency of the Council of the EU from January to June 2019. The Council of the European Union is the institution where the governments of the EU Member States defend their own country’s national interests in the negotiation of the legislative and non-legislative files. Every EU Member State has the obligation to hold the Council Presidency, which changes every six months.
About the CoR
The European Committee of the Regions is the voice of regions and cities in the EU, aiming to reduce the gap between EU institutions’ work and EU citizens. It is composed of more than 350 local and regional elected representatives from across the EU and advises on new laws that have an impact on regions and cities (which is 70% of all EU legislation).
SPONSORS
We are grateful to our sponsors for their generous support of this event.


CONTACT US
Follow this page as well as our Facebook page and Twitter account to see regular updates on this event.
You can get in touch with us at: info@safestroke.eu



 “I set a sign.”
“I set a sign.” The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters.
The German Stoke Foundation launched their new website at the end of October (World Stroke Day). Thanks to the modern design, the information presented on the new website is now easier to find for stroke-patients and their relatives as well as for experts and supporters. The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke.
The project “STROKE OWL” started in 2017 and is financed by the German “innovation fund” with seven million euro. OWL stands for “Ostwestfalen-Lippe”, the region in Germany where the German Stroke Foundation is based. The foundation wants to prove that continuous case management is able to improve the situation of stroke-patients and reduce the risk of a second stroke. The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning:
The German Stroke foundation is looking forward to 2019. Some of the events and projects the team is planning: