Sep 23, 2019
Written by Prof. Anita Arsovska, MD, PhD, FESO, SAFE Board member
The Management Committee Meeting of IRENE COST Action took place in Chisinau, Moldova, 16th-17th of September 2019, hosted by Prof. Stanislav Groppa, attended by 46 delegates from 26 countries (several SAFE members), chaired and co-chaired by Robert Mikulik and Natan Bornstein, respectively.
Based on the principles of ESO-EAST platform which was created by Prof. Valeria Caso and the efforts of the Steering Committee, and also formation of RES-Q database, IRENE stands for Implementation Research Network in Stroke Care Quality. ESO and SAFE have been working together more closely in the previous years, especially since signing of the Memorandum of Understanding during ESOC 2017 in order to improve stroke care in many European countries. Effective methods for stroke treatment exist; however the implementation of these treatment methods is very low and therefore constitutes the most challenging problem in current stroke management. In many countries and many hospitals, patients do not receive effective treatment because implementation framework is missing.

Image credits: Yuriy Flomin; Source: Facebook
During the meeting, Veronika Svobodova (Grant Manager) stated that the core activity of the IRENE COST Action is to improve public health through; a) Networking which will facilitate understanding of contextual factors, in between-country differences in innovation-values fit and implementation climate, b) a quality registry that will provide a cohesive picture of the implementation of stroke treatments; followed by c) the dissemination of results to the main stakeholders (e.g. hospitals and Ministries of Health) to implement new mechanisms to improve the outcome of stroke.
The IRENE COST Action will be conducted mainly in European countries where the burden of stroke is higher, while quality of stroke care is lower and resources for healthcare are less developed compared to other European countries. IRENE COST Action will alleviate disparities in stroke care and improve outcomes after stroke. IRENE COST Action is a platform for networking with defined goals.

Image credits: Yuriy Flomin; Source: Facebook
One of the main Capacity Building Objectives is to develop tools for increasing professional skills and knowledge of IRENE COST and sharing best practice between COST members during the IRENE COST Action period. Actually, the first IRENE COST Training school “Communicating scientific data and results to the public” will be organized by SAFE’s Vice-President Markus Wagner in March next year, in his hometown Gütersloh, Germany where together with other experienced speakers he will share his rich experience and knowledge within the German Stroke Foundation in terms of improving the communication of science to the pubic and journalists. During the first day of the Training School- Principles, examples, tips and tricks in Scientific communication will be shared and during the second day lectures regarding Implementing of Stroke Services (experience from Germany), Communication and campaigning, Certification and Quality indicators will be held, presenting the the political work of SAFE in Brussels using data from the Burden of Stroke / Economic burden of Stroke and Stroke Action Plan For Europe (SAFE/ESO).
Overall, the two days intensive meeting was an excellent opportunity to meet with colleagues, make plans for future collaboration, exchange knowledge, and also and great inspiration to continue to work in order to improve the quality of stroke care in each country involved. All delegates enjoyed the warm hospitality of Prof. Stanislav Groppa and his team and were delighted by the charming city of Chisinau and its natural beauties.
Sep 20, 2019

Kjell Holm, General Manager of the Swedish stroke association STROKE-Riksförbundet
The number of people suffering strokes in Sweden is declining with 600 fewer cases in 2017 compared to the year before. On top of that, many people think that Scandinavian countries have everything perfectly set up when it comes to stroke and the entire stroke care pathway, from prevention to life after stroke. This week, SAFE spoke with Kjell Holm, General Manager of the Swedish stroke association STROKE-Riksförbundet, who told us about some room for improvement.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
KH: A system for follow-up after stroke. Many stroke-survivors are not provided with rehabilitation after stroke and don’t know where to apply for it. The Stroke-survivor and carers also need a healthcare contact after stroke to talk about their needs and new situation.
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
KH: The Swedish Stroke association focuses on and highlights on a system for follow up after stroke for all patients. One tool is the “Post Stroke Check List” and an individual plan for the follow up and rehabilitation.
SAFE: Please tell us more about your organisation.
KH: The Swedish Stroke association started in 1983 and has now 9000 members and 83 associations/clubs all over Sweden. We also have a Stroke fond that contributes to stroke science with 3 000 000-4 500 000 Kronor each year. We are included in providing stroke education for the staff in the stroke healthcare. We distribute a lot of stroke information as books, films, papers, leaflets, website, pod, YouTube, twitter. We also write articles and have meetings with the politicians and decision-makers.

Sep 17, 2019
A useful repository for reliable and easy to use information on 10 modifiable stroke risk factors translated to Polish, Spanish, Portuguese, Russian and French.
Brussels, 17/09/2019: A SAFE-owned website on stroke prevention and modifiable stroke risk factors goes live today at www.strokeprevention.info in five additional European languages: Polish, Spanish, Portuguese, Russian and French.
Increasing the number of languages on this website will allow greater accessibility of its content for millions of people who speak these languages, alongside the website’s original language, English.
Around 17 million strokes occur worldwide each year, despite compelling evidence that it is a largely preventable condition. Stroke shares risk factors with other cardiovascular diseases (CVDs) and with many other non-infectious, or non-communicable diseases (NCDs). Addressing stroke risk factors requires both individual and society level interventions – addressing lifestyle and medical issues. This knowledge motivated SAFE to create the website www.strokeprevention.info. The aim of this website is to inform and inspire people to take individual interventions, such as giving up smoking or taking better control over their blood pressure and take an active role in preventing stroke.
Based on the INTERSTROKE study’s findings, ten modifiable risk factors are responsible for 90% of strokes. This website collates all relevant information on the most common risk factors such as: hypertension, physical activity, diet, obesity, smoking, cholesterol, heart disease, alcohol, stress and diabetes. In addition to being written in a lay-friendly language, all website information is in a format appropriate for people with disabilities.
This website is developed and owned by Stroke Alliance for Europe (SAFE), which retains full editorial control over the content.
The original version of this website was originally launched in English in 2018 and was supported by an educational grant from Amgen. The translation into five European languages was enabled by Boehringer Ingelheim in 2019. SAFE is grateful to the generous supporters of its work, which enables important stroke prevention information to reach wider audiences.
About SAFE
The Stroke Alliance for Europe (SAFE) a non-profit-making organization formed in 2004. It is the voice of stroke patients in Europe, representing a range of patient groups from 30 European countries. SAFE’s goal is to decrease the number of strokes in Europe by advocating for better prevention, access to adequate treatment, post-stroke care and rehabilitation.
Sep 13, 2019
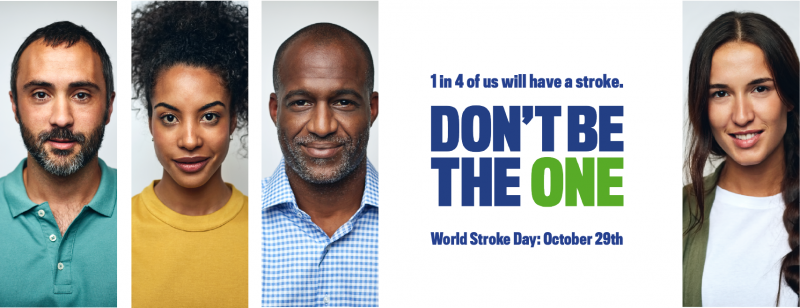
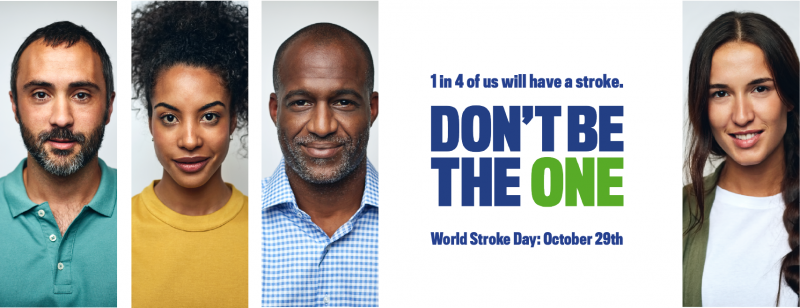
World Stroke Day 2019 to focus on stroke risk and prevention
The World Stroke Organization has announced the theme for World Stroke Day 2019. With a focus on stroke prevention, the ‘Don’t be the One’ campaign aims to raise awareness of our individual lifetime risk of stroke and to equip as many people as possible with potentially life-saving prevention information and tools.
The rationale for the campaign message is the recent WSO analysis of the Global Burden of Disease, which shows that globally the lifetime risk of stroke has risen and now stands at 1 in 4. Combined with the Interstroke findings that showed around 90% of strokes are linked to a small number of easily addressed risk factors, the potential impact of public understanding of stroke risk and prevention awareness is clear.
Speaking about the World Stroke Day campaign theme, World Stroke Organization Vice President and Campaign Committee co-Chair, Sheila Martins said ‘For me the 29th October is always such an exciting day for the stroke community – it’s the one day of the year that we can come together globally and to make as many people as possible aware of stroke. This year our message When it comes to stroke, think prevention – Don’t be the one.’ is relevant and essential to everyone and we look forward to seeing the stroke community taking up the campaign in countries around the world!’
Co-Chair Deidre De Silva and a leading awareness campaigner Singapore ‘Our team strived to deliver a campaign that will resonate with diverse populations around the world. Stroke is not prevented by hoping it will never happen to you. The campaign encourages everyone to be proactive by understanding their stroke risk and taking the steps to prevent stroke and its devastating consequences.’
World Stroke Day Campaign Resources
A campaign guide for members and the public will provide guidance on how to join the global prevention awareness effort. This will be available from the revamped World Stroke Day website. Members and partners will have access to campaign resources including the campaign video, gifs, editable posters, infographics, social media posts and translated prevention factsheets.
Stroke Riskometer
The Campaign team is also working in close partnership with the Stroke Riskometer team at Auckland University of Technology to promote the WSO endorsed Stroke Riskometer as a tool to understand individual stroke risk and to identify individual risk factors. Riskometer users will be encouraged to conduct their own risk assessment and to share the app on social media tagging four friends. If one person who is tagged downloads and uses the app, they will have free access to an app upgrade that will support them to take appropriate action to reduce their stroke risk.
The Campaign Committee is reaching out to members and supporters asking you to mobilise your global stroke ambassador and influencer network to help us get our potentially life-saving message to as many people as possible.
Please contact awiseman@kenes.com to dicuss further.

Sep 13, 2019
“Patients’ families have even less support than patients themselves and are often left alone to manage their life and organise the life of their family member with stroke.” said Milan Čuček, President of the Slovenian Stroke Support Organisation and the Vice President Tatjana Erjavec added “It is challenging for carers to assist them with integration into relevant social networks. Stroke support organisation is currently trying to bridge this gap.”
This week we are investigating what is the main after-stroke problem from the patients’ perspective in Slovenia.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
Stroke Care starts in hospitals and majority will have multidisciplinary teams to take care of stroke survivors. Patients with severe disabilities and rehabilitation potential will continue their rehabilitation either at the Rehabilitation Institute or in dedicated Spa’s around Slovenia. This process takes up to 6 weeks. Nowadays, stroke survivors have the possibility for ongoing visits to neurologists. Systematic rehabilitation support is, however, lacking.
Majority of stroke survivors return to their homes with limited access to further rehabilitation programmes. There is a possibility for subsides home help for maximum 20 hours per week and if medical condition requires, also visits from nurses. Primary level provides physiotherapy across Slovenia, but only on the outpatient basis and in limited amount. Occupational therapy is only available in three primary level institutions around country and it is delivered in patients’ homes. Psychology and speech therapy is virtually not available in the community. Private services are possible and this creates imbalance considering access to health services in favor of those who are financially stronger. Majority of stroke survivors are retired and with lower pensions and have therefore limited access to private therapies. In addition, it is observed that central Slovenia and bigger cities have better long-term support comparing to rural parts around country and North West part of Slovenia.
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
Slovenia is a small country with population of 2 million and a good network of primary care. So far, primary care provides social service, limited access to physiotherapy and limited occupational therapy services. Ministry of Health has appointed special group, dealing with organisation of long term support for stroke survivors and creating a document for local long-term multidisciplinary stroke care. In addition, the legislation, dealing with long-term home care also includes multidisciplinary care. The challenge remains implementation of both, related to provide enough financial resources.
Slovenia has well developed Spa rehabilitation. Stroke survivors have an access to Spa rehabilitation in acute stage. Regular access to Spa rehab in sub-acute and chronic stage is not guaranteed by insurance. Stroke Support Organisation highly value this rehabilitation programs for stroke survivors and their relatives and therefore enables it for 100 members per year, being aware that this is not enough.
Ongoing support for carers is essential and it could be organised via educational sessions, self-help groups, organised respite care.
Patient organisations, providing social and health support in public interest, should have an ongoing financial support. Accessing finances via public calls requires professionally that can hardly work voluntarily all the time.
SAFE: Please tell us more about your organisation.
Slovenian Stroke Support Organisation is going to celebrate 30 years of its existence. It operates through 22 stroke clubs around Slovenia and it has 3000 members; mainly stroke survivors and relatives, but also few professionals (volunteers) and other supporters. Leaders of local stroke clubs are stroke survivors. Registered is as a Humanitarian organisation working in public interest. Main financing comes on annual basis from National lottery (FIHO). Additional income comes from local municipalities where clubs are operating, public calls for NGOs, memberships, donations and sponsorship, collaboration in research projects.
Main activities are enabling long-term rehabilitation support via SPA’s, organised physiotherapy in stroke clubs, sport activities, organized exercises (Nordic walking), organized walks. In addition, social networking, educational sessions for stroke survivors and families, organised creative workshop. In last years we provide workshops about self-care and aphasia group. Each year is organised National gathering and this year it will be in Postojna cave for over 370 members. Twice per year, journal KAPNIK is published and the website is constantly updated.
With respect to promotion we organize several events, including traditional walk around Ljubljana, for the European stroke day. Several events are also organized around World Stroke Day. The WSO has given award to our SSO for the best campaign in high income countries for year 2018.